How did COVID-19 impact stroke rehabilitation?

Authors: Ioana Stanescu, Oana Vanta
Keywords: COVID-19 impact stroke rehabilitation, COVID-19 infection, stroke outcome, health care, pandemic
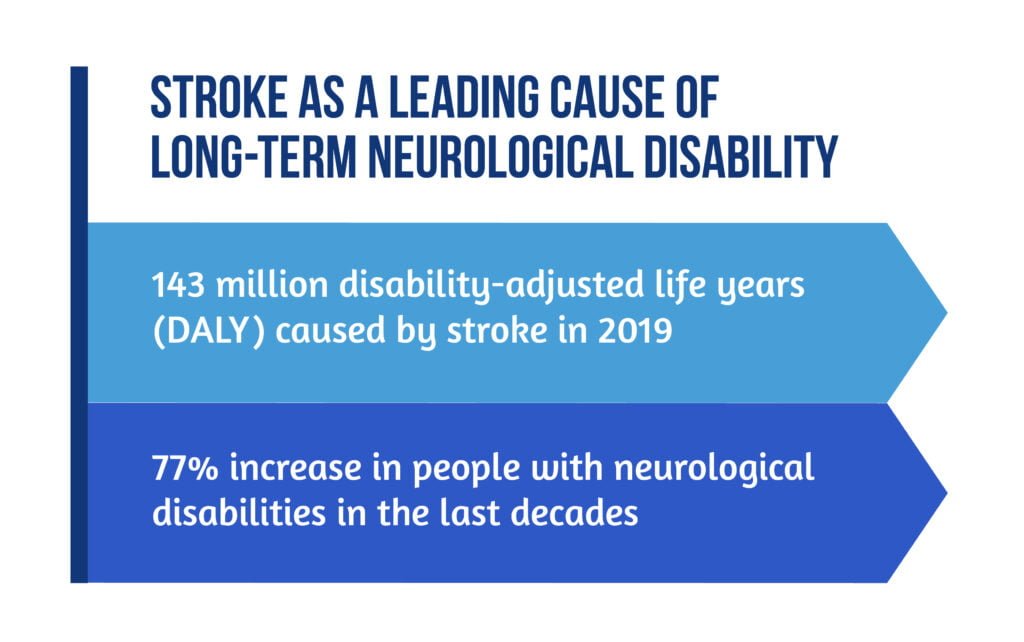
What is the trend for stroke incidence and disability in the last decades?
Worldwide, stroke is the third cause of death and disability combined. The burden of stroke has increased in the last 20 years, with 70% in incidence and 43% in mortality [1].
According to the World Stroke Organization (WSO), there are geographical inequalities in stroke mortality, with higher rates in lower-income (LIC) and lower-middle-income countries (LMIC) [1]:
- Poorer stroke outcome in LIC and LMIC
- 86% of all stroke deaths belong to LIC and LMIC.
Stroke is a leading cause of long-term neurological disability [2,3], as showcased in Figure 1.
What changed in stroke outcomes during the COVID-19 pandemic?
Healthcare patterns have changed during the COVID-19 pandemic. Stroke care was negatively impacted, and patients’ outcomes have worsened. Also, the SARS-COV-2 infection is an additional risk factor for ischemic stroke through the mechanism of arterial and venous thrombosis and hypercoagulability state, which could probably increase stroke incidence [4].
The factors that contributed to impaired stroke prognosis during SARS-COV 2 pandemic and lockdowns are presented below.
Related to COVID-19 infection itself:
- higher incidence of thromboembolic mechanisms in stroke, proved by large vessel occlusions and simultaneous involvement of different vascular territories
- increased severity of stroke attributed to COVID-19 (higher NIHSS score)
- younger age of patients with COVID-associated stroke than of patients with stroke without COVID-19
- the higher mortality rate of stroke patients with concurring COVID infection during hospitalization, despite appropriate treatment in the acute phase
- SARS-COV-2 infection in stroke patients increases the overall mortality rate [4–5].
Related to the healthcare system:
- reorganization of emergency departments and stroke care services to deal with the influx of COVID patients
- acute care limitations due to beds and medical staff reassignment
- fewer stroke beds
- relocation of stroke physicians
- decrease in the number of stroke patients who access medical services:
- avoidance of emergency service access for patients with mild stroke symptoms (fear of acquiring COVID)
- patients living alone (in isolation) may not be aware of stroke symptoms and do not seek medical attention
- fewer patients are diagnosed with stroke
- shorter duration of inpatient stay for stroke treatment
- a greater level of disability at discharge [5].
How did COVID-19 impact stroke rehabilitation?
Multidisciplinary rehabilitation in stroke is effective in reducing functional impairment. Early access to rehabilitation is critical and should be facilitated in early stroke phases and in vulnerable patients. Stroke patients require coordinated action from the rehabilitation team during acute hospitalization, inpatient rehabilitation, and community-based care [6].
The COVID-19 pandemic had a significant impact on rehabilitation care provided to stroke patients:
- Minimal or no early rehabilitation treatment is provided during acute hospitalization
- Changes in the discharge of stroke patients in post-acute care:
- fewer patients discharged to skilled nursing facilities
- more patients discharged at home
- the same number of patients admitted to inpatient rehabilitation
- Lack of follow-up rehabilitation plans after discharge
- Delays in bridging the inpatient to the outpatient rehabilitation program
- Lack of support in the community and home-based rehabilitation care:
- reduction of in-home health services for stroke patients
- delays in providing community- and home-based rehabilitation
- additional roles for family members in care and rehabilitation
- Increased stress for families and caregivers of discharged stroke patients
- Decreased physical access of patients in community centers for training and socialization (support groups)
- Inadequate training of caregivers or family members for providing appropriate care and essential rehabilitation
- the inability of family members to be involved in patient care during hospitalization (visits suspended)
- Limited communication with physicians and healthcare professionals
- Difficulties in accessing technology-assisted rehabilitation
- Increased risk of undetected complications in stroke survivors
- Challenges in treating communication disorders wearing a mask
- Increased cognitive impairment caused by social isolation
- Increased predisposition to a more sedentary lifestyle due to the lockdown
- Decreased family financial resources
- Increased anxiety and depression in patients and caregivers [5–6].
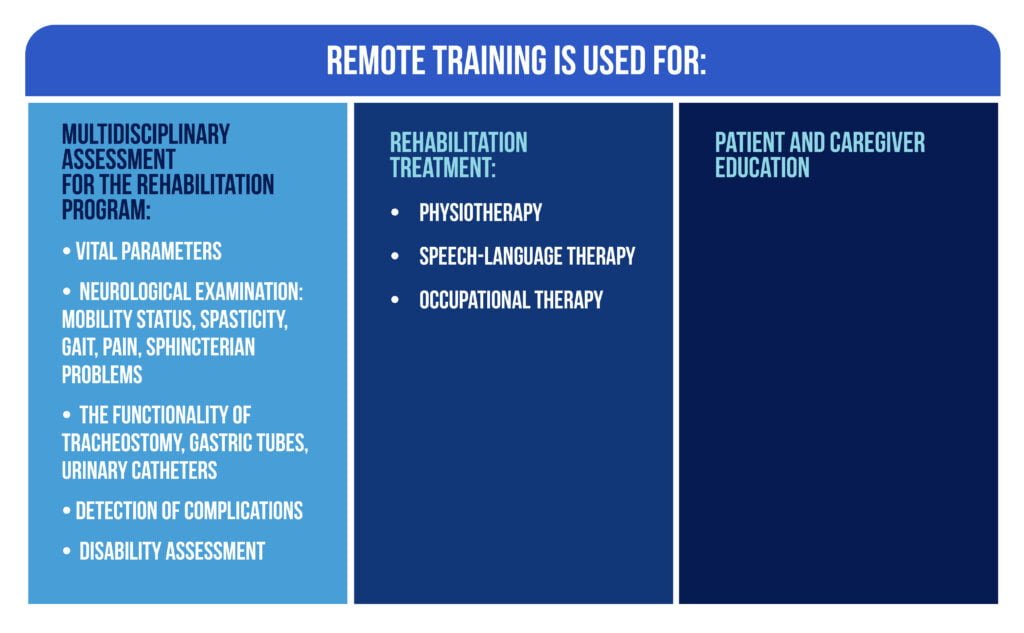
Is telerehabilitation a solution to improving patient care during the COVID pandemic?
Stroke patients discharged with neurological disabilities need to be involved in a rehabilitation program as soon as possible and to access inpatient, outpatient, or home-based rehabilitation services. Telerehabilitation has been proven to be an effective strategy for overcoming pandemic restrictions [7]. Remote training assures the continuum of care of stroke patients. Its uses are described in Figure 2.
There are some barriers to method implementation during the pandemic, such as the ones described in Figure 3.
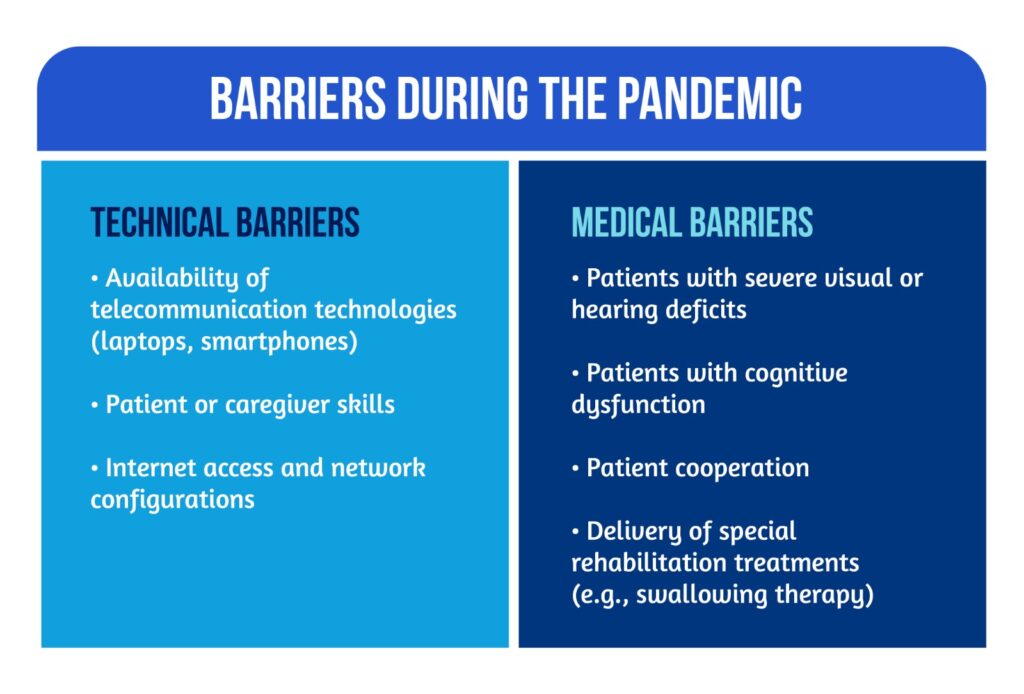
Despite the limitations, telerehabilitation is an accessible and widely available treatment method during pandemic restrictions [7].
What are the conclusions on COVID-19 impact stroke rehabilitation?
The COVID-19 pandemic negatively impacted stroke care, highlighted by the fact that stroke patients accessed healthcare services less often and had more severe neurologic deficits. Although stroke patients were discharged with severe disabilities, delayed rehabilitation plans were implemented, and recovery outcomes were less favorable.
Patients’ access to community-based and home-based rehabilitation facilities is delayed and complicated, with interruptions and delays in the patient’s training program. Due to this, a comprehensive approach considering the involvement of caregivers or additional tools such as telerehabilitation should ensure the best care for the patients.
For more information on neurorehabilitation, visit:
- How can music improve stroke recovery?
- How does gender influence stroke and neurorehabilitation?
- Adequately Targeted Brain Stimulation in Post-Stroke Motor Rehabilitation
References
- Markus HS. The inequality of stroke in 2022: The impact of geography, COVID-19, and time of day, on stroke outcomes. Int J Stroke. 2022;17(1):7-8. doi: 10.1177/17474930211069203
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Neurology 2021. doi: 10.1016/S1474-4422(21)00252-0.
- Kim J, Thayabaranathan T, Donnan GA, et al. Global Stroke statistics 2-19. Int J Stroke 2020;15:819-838, doi: 10.1177/1747493020909545
- Burns SP, Fleming TK, Webb SS, Kam ASH et al. Stroke Recovery During the COVID-19 Pandemic: A Position Paper on Recommendations for Rehabilitation. Arch Phys Med Rehabil. 2022;103(9):1874-1882. doi: 10.1016/j.apmr.2022.04.004.
- Nannoni S, de Groot R, Bell S, Markus HS. Stroke in COVID-19: A systematic review and meta-analysis. Int J Stroke. 2021;16(2):137-149. doi: 10.1177/1747493020972922.
- Lucas L, Gordon S, Heyes R. Impact of COVID-19 on the stroke rehabilitation pathway: multidisciplinary team reflections on a patient and carer journey from acute to community stroke services. BMJ Case Rep. 2021;14(11):e245544. doi: 10.1136/bcr-2021-245544.
- Srivastava A, Swaminathan A, Chockalingam M, Srinivasan et al. Tele-Neurorehabilitation During the COVID-19 Pandemic: Implications for Practice in Low- and Middle-Income Countries. Front Neurol. 2021;12:667925. doi: 10.3389/fneur.2021.667925.