How does gender influence stroke and neurorehabilitation?

Authors: Irina Benedek, Oana Vanta
Keywords: stroke, genders, risk factors, post-stroke disabilities
How does gender influence stroke?
What is a stroke? – Definition, epidemiology, and risk factors: general considerations
Definition: The term “acute stroke” or “cerebrovascular attack” refers to a sudden onset of focal or global neurological deficits due to interruption of blood flow in a specific vascular territory supplying the brain [1].
Epidemiology: 60% of strokes happen outside hospitals in the United States, where they also represent the fifth most common cause of death. Generally, a stroke occurs on average every 40 seconds, and one stroke-related death happens every 4 minutes [1]. Therefore, this pathology remains the leading cause of morbidity and disability worldwide, despite recent progress in neurorehabilitation.
Several different etiologies might cause a stroke. Some of the most common risk factors for developing an ischemic cerebrovascular accident include those showcased in Figure 1.

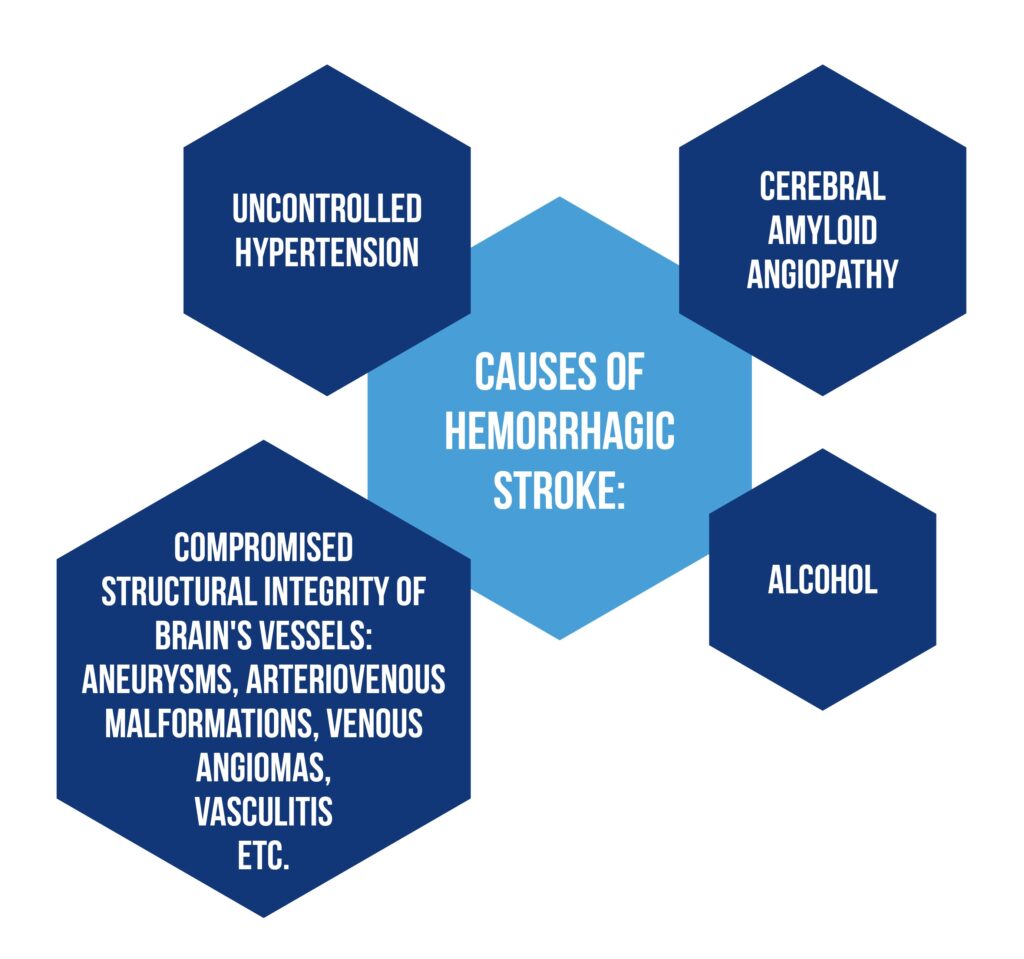
Regarding hemorrhagic stroke, which represents 15% of all strokes, the most common etiology is uncontrolled hypertension. The most common etiologies are described in Figure 2 [1].
How does gender influence the onset of a stroke?
Women have a 1 in 4 chance of developing a stroke after 25 years old, making them more at risk of having a cerebrovascular accident during their lifetime than males. Nevertheless, stroke rates are more significant in men than women throughout midlife. Moreover, the risk increases in women beginning with the eighth decade. Incidence ratios of females to men throughout the reproductive years are still contradictory. Consequently, further investigation is required to establish the causes of the reversed risk ratio for women after menopause and whether variables affecting vascular dysfunction, including sex hormone levels and biological age, could represent potential therapeutic targets for stroke prevention [2].
Figure 3 showcases the prevalence of risk factors for stroke by gender.
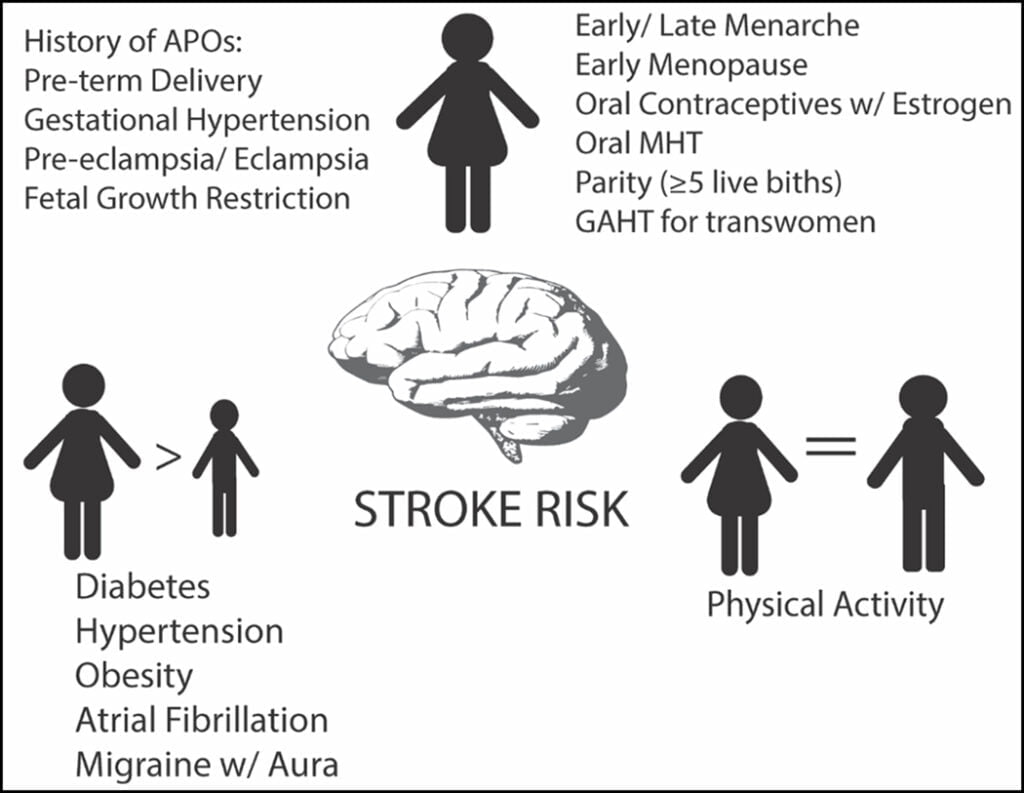
Recent research is inconclusive as to whether endogenous levels of age-varying sex hormones (e.g., testosterone, estradiol, and sex hormone-binding globulin) are independently related to stroke [2].
Does gender influence stroke risk factors?
Diabetes and hypertension are two major modifiable risk factors that seem to manifest differently depending on gender.
- Diabetes, especially type 1, has a stronger correlation with the incidence of ischemic stroke in women compared to men. Even after accounting for therapy with oral medication or insulin, the risk for ischemic stroke starts to increase at lower fasting blood glucose levels for women than for men. More research is required to comprehend the biological reasons driving these gender disparities fully. For the time being, regular diabetes screening is advised [2].
- When referring to hypertension, recent data from international cohorts show a stronger association between hypertension and the risk of ischemic stroke in women compared to men, despite some prior data suggesting no consistent differences in this regard. Sexual dimorphism in the contribution of blood pressure to cardiovascular disease and stroke has been supported by longitudinal data in the United States, which show that women’s blood pressure rises more quickly than men’s, starting with the third decade of life [2].
- In both genders, a greater risk for all types of stroke is related to a high body mass index, clinical obesity (body mass index, 30 kg/m2), and a larger waist-to-hip ratio, with a stronger association in women than in men. Obesity and hemorrhagic stroke have a more complicated link; there is some evidence that women may be protected, but studies also show that this varies by gender [2].
- According to statistics, the risk of stroke and all-cause mortality is more significant in women with atrial fibrillation than in men, making it a modifiable risk factor for both sexes. The risk of recurrent stroke occurrences is notably high in women over 65 who suffer atrial fibrillation [2].
Do women possess a higher risk for post-stroke disabilities than men?
While the death rate does not differ between genders, women, in contrast to men:
- are older at the time of stroke onset
- have worse functional outcomes at 3 months and 1 year than males.
The female gender was a predictor of poor functional outcome at 3 months and 1 year following a stroke, even after adjusting for various confounding factors such as age, disease severity, and risk factors. These findings imply that women often have a longer lifespan after an acute stroke but experience more disability than men [3].
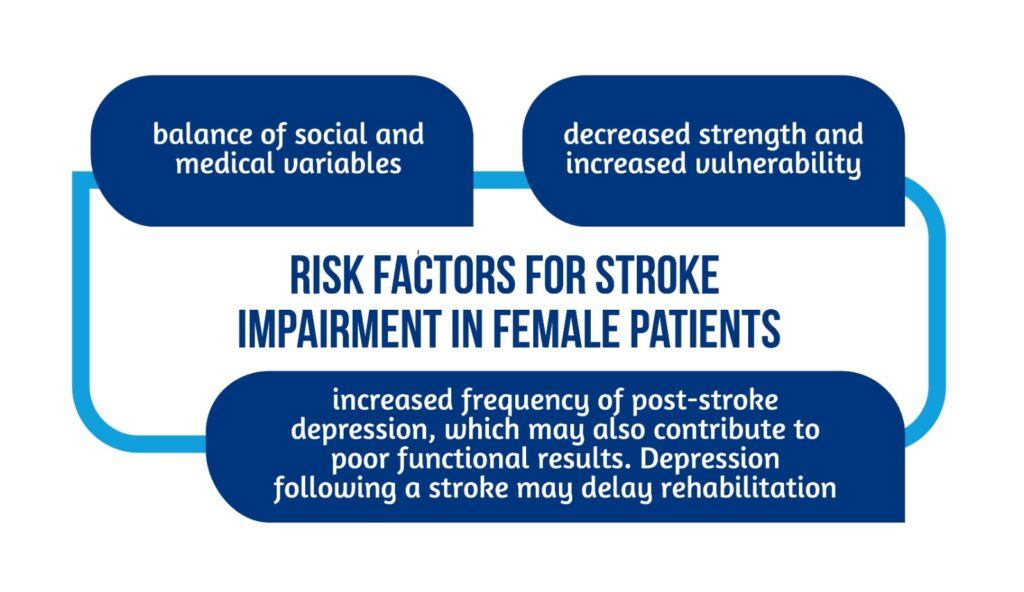
Previous studies have revealed that women tend to experience lower functional results after stroke, providing explanations for this finding. According to research, the following factors contribute to worse functional results for women:
- lower preadmission functional condition
- less social support—more women than men are widowed and live alone [3].
Gender is a strong predictor of impairment and handicap for women who suffered a stroke due to the factors in Figure 4 [3, 4].
The mortality rate from stroke has produced a variety of outcomes [3]:
- Between 1999 and 2004, the death rate in the USA was greater for women than for men between the ages of 35 and 85 but lower for the other age groups
- Mortality rates from all causes were higher for women than for men, according to certain research, but after controlling for confounding variables, males had the higher mortality rates as cardiovascular disease was more common in men.
- Women had a greater risk of mortality from any cause at discharge than men, especially to their older age and more severe stroke symptoms upon admission.
What are the conclusions?
There have been reports of gender variations in stroke subtypes and risk factors in the past. According to certain research, female patients were more likely to experience atrial fibrillation and cardioembolic infarction stroke subtypes [5].
Women were more likely than men to have the following risk factors:
- hyperlipidemia,
- hypertension,
- cardioembolic sources [6].
However, small-vessel occlusion, a stroke subtype, was less commonly observed in female patients. The limited sample size, geographical features, or the constraint on using a single hospital-based registry may all be contributing causes to the variations in the distribution of stroke risk factors and subtypes; therefore, more research is needed [3].
There have been reports of gender variations in stroke subtypes and risk factors in the past; taking into account all the data, women are more likely to experience worse outcomes after a stroke; therefore, the neurorehabilitation process can take longer and less efficient than for men. Consequently, the need for developing specific gender management protocols should be considered.
For more information on stroke neurorehabilitation, visit:
- Rehabilitation of non-fluent aphasia patients
- SENSe: Assessing neurorehabilitation’s impact on the somatosensory function in stroke patients
- Can gaming therapy impact post-stroke rehabilitation?
References
- Tadi P, Lui F. Acute Stroke. [Updated 2022 Jun 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535369/
- Rexrode KM, Madsen TE, Yu AYX, Carcel C, Lichtman JH, Miller EC. The Impact of Sex and Gender on Stroke. Circ Res. 2022 Feb 18;130(4):512-528. doi: 10.1161/CIRCRESAHA.121.319915.
- Kim JS, Lee KB, Roh H, Ahn MY, Hwang HW. Gender differences in the functional recovery after acute stroke. J Clin Neurol. 2010 Dec;6(4):183-8. doi: 10.3988/jcn.2010.6.4.183.
- Di Carlo A, Lamassa M, Baldereschi M, et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke. 2003;34:1114–1119. DOI: 10.1161/01.STR.0000068410.07397.D7
- Roquer J, Campello AR, Gomis M. Sex differences in first-ever acute stroke. Stroke. 2003;34:1581–1585. DOI: 10.1161/01.STR.0000078562.82918.F6
- Oh MS, Yu KH, Rho JK, Lee BC. Korean Stroke Registry Study Group. Gender differences in the motality and outcome of stroke patients in Korea. Cerebrovasc Dis. 2009;28:427–434. DOI: 10.1159/000235986









