Robotic-aided therapy in motor recovery after stroke

Author: Livia Popa, Oana Vanta
Keywords: exoskeletons, EMG, EEG, human-machine interface, ADL, neurorehabilitation, motor assistance, emerging technologies
Robotic-aided therapy in motor recovery after stroke – is it possible?
Stroke affects one in five hundred people each year and is, using a consequence, the leading cause of long-term disability, with a very severe limitation in day-to-day activities [1].
Physical therapy and exercise induce changes in cortical reorganization, depending on the residual neuroplasticity, thus making motor recovery possible.
The significant motor determinants of recovery are showcased in Figure 1.
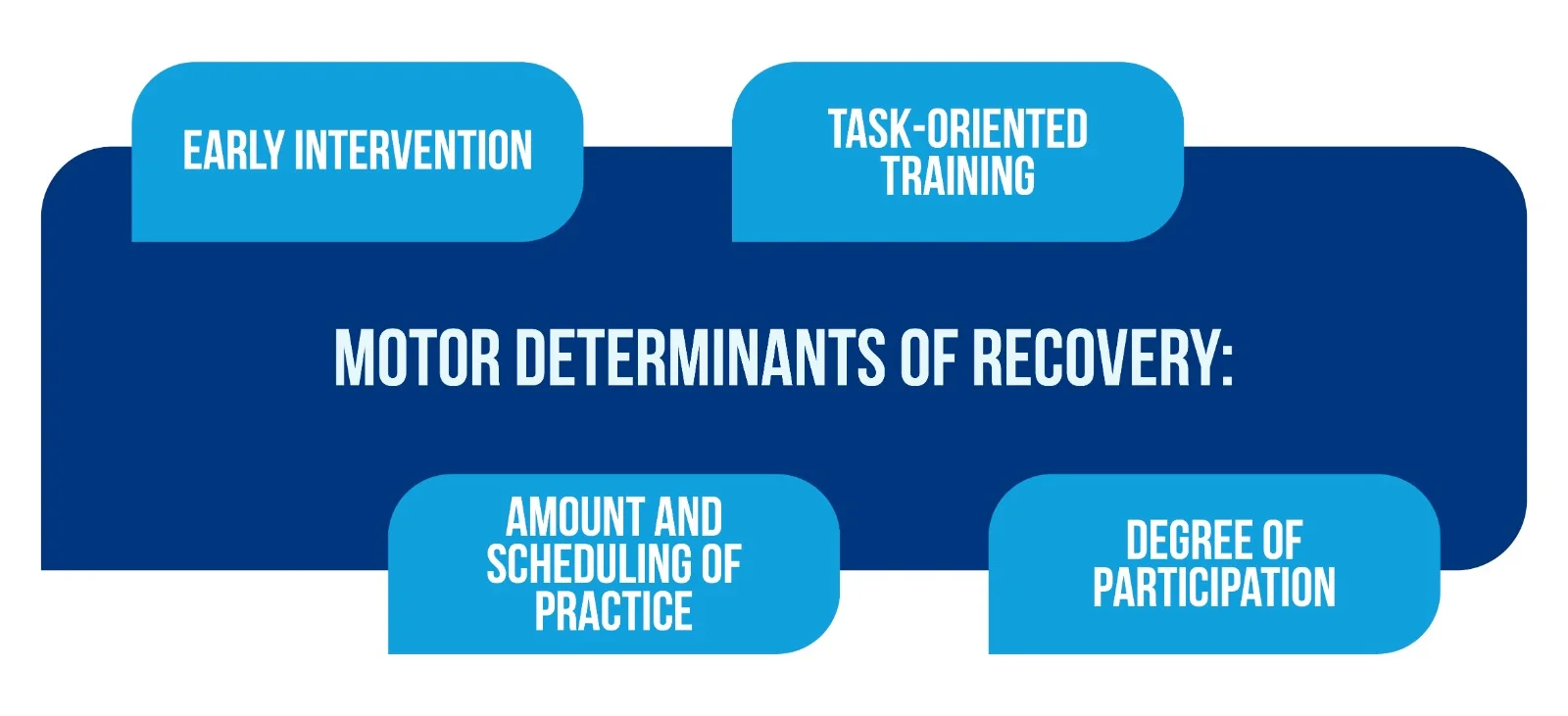
Task-oriented training, in particular, consists of the repetitive skill-related practice of functional tasks. This kind of training has been clinically tested in stroke patients for:
- locomotion
- balance
- arm-hand function recovery
- motor control
- strength.
The fundamental principle behind motor learning is that the amount of practice determines the degree of performance improvement. At the same time, the degree of patient participation is of utmost importance because active and strong involvement and volitional effort are crucial for inducing cortical reorganization [1].
Is robotic-aided therapy more effective than conventional physical therapy?
While conventional neurorehabilitation does not seem to significantly impact impairment beyond spontaneous biological recovery [1], robotics has proven to be an enabling technology of major support in enhancing the healing process and minimizing functional disability.
Robots are ideal instruments in supporting neurologists and therapists to confront the great challenges of the neuro-rehabilitation process, as robotic-aided therapy has been observed to be more effective than traditional physical therapy due to the:
- high intensity of exercise,
- better movement controllability,
- measurement reliability.
At the same time, compared to traditional physical therapy, rehabilitation robots can provide training:
- at a much higher dosage (number of practice movements);
- at a much higher intensity (number of movements per unit time).
What are robotic exoskeletons?
Robotic exoskeletons have been revealed as a rehabilitation tool with alleviating potential in several locomotion issues. They are robotic units that can be worn by patients and can assist them in neuromotor rehabilitation. Patients with paraplegia following stroke, peripheral neuropathies, or spinal cord injury can benefit from autonomous walking provided by wearable devices, like upper and lower limb robotic exoskeletons, which most commonly actuate the knees hips and ankle joints [1].
A wearable device is considered an active mechanism that:
- is essentially anthropomorphic
- can be” worn” by its operator
- fits closely to the operator’s body
- works in sync with the operator’s movements [1].
For example, the Alex 2 exoskeleton, which can be seen in Figure 2, has been developed with exceptional potential in kinematics and actuation on 4 levels of freedom, as it was developed with the integration of elastic tendons to ensure mechanical conformity.

Exoskeletons offer a considerable degree of independence in medical centers and communities and an improved level of physical activity due to their essential role in supporting the patient’s body weight and generating symmetrical gait patterns [2]. As shown in Figure 3 [3], the exoskeletons used in medical centers are not portable devices, but with their help, even tetraplegics come to move.

How are robots helpful in motor recovery?
Therapy assisted by robotic tools in upper limb rehabilitation has been shown to improve motor capability and motor-task performance significantly. In more specific terms, patients who are assisted by electromechanical tools in their training after stroke have more chances to:
- improve their generic activities of daily living (ADL);
- improve arm function.
Lower limb exoskeletons provide patients with independence from a wheelchair, having a positive impact on their life quality, by:
- increasing freedom to move and perform ADLs;
- improving internal organs’ functioning and general health status.
While they make a great difference in disabled patients’ daily lives, few exoskeletons provide user balance by themselves; most of the devices still have to be completed by use of crutches for balance to be obtained, and here lies the need for further research and improvement in motor assistance devices [1].
Which biosignals are frequently used to develop robotic aids?
It is easily understandable that passive movement driven by a robot along a trajectory, without the active involvement of its user, does not result in learning – as noted before, a volitional effort is needed to induce cortical reorganization. This is why the fundamental aspect of motor learning is the patient’s degree of participation in the robotic training. Producing devices that can recognize the patient’s intention in rehabilitation tasks has been a great challenge for robotic tools, and the effective approach to this matter is based on using bio-signals.
The most frequently used bio-signals in rehabilitation are:
- Electromyography (EMG), which is the electrical manifestation of the neuromuscular activation associated with a contracting muscle and collected from preserved or moderately impaired muscles;
- Electroencephalography (EEG) is the electrophysiological monitoring method of recording electrical activity in the brain [1].
What kind of assistance do the EMG-based interfaces provide?
EMG signals represent a control interface for robots; by encoding brain-generated information, they can contain data regarding planning and execution used to control artificial systems [4].
EMG-based robot control can be considered a natural way of developing assistive controllers able to provide assistance calibrated by the level of muscle activation [1] through:
- Triggered assistance, in which the patient initiates movement without help while the robot assesses ongoing performance and takes full control when the task is not fulfilled;
- Adaptive control strategies, in which the EMG signal’s power directly controls the device inside the robot that produces motion [4].
What kind of assistance do the EEG-based interfaces provide?
Some systems use brain signals as conductors of external devices, with no other actual movements of the body to initiate the devices, known as Brain-Computer Interface (BCI) or Brain Machine Interface (BMI).
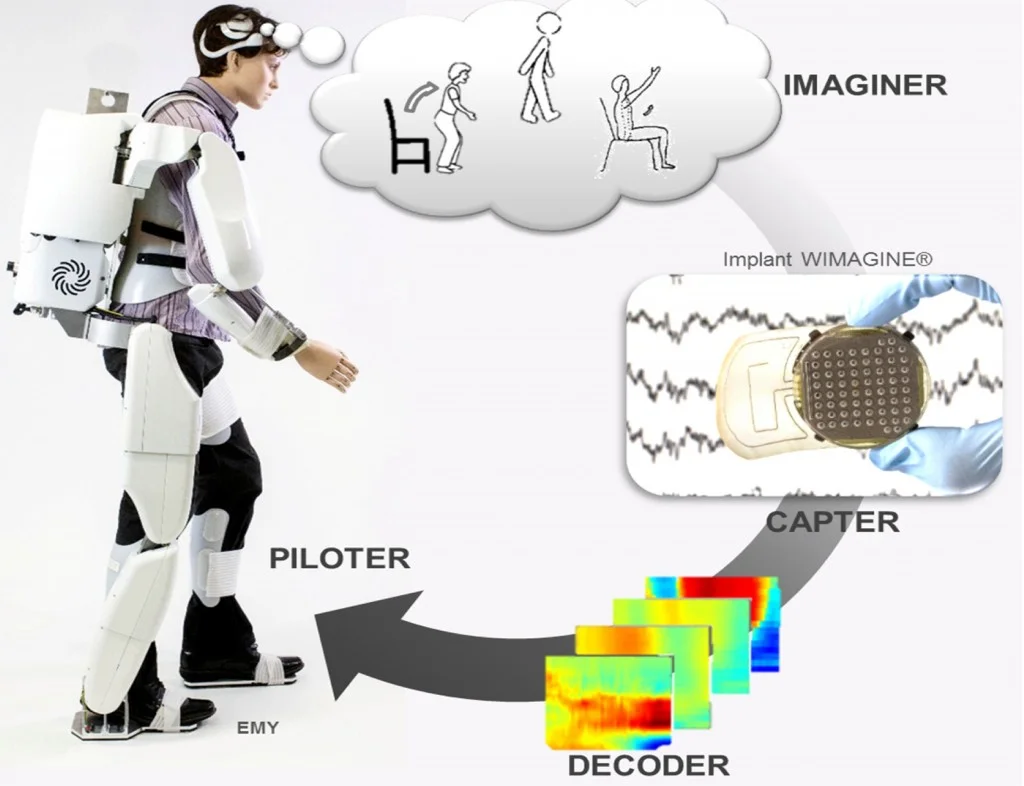
The user’s brain activity is recorded and decoded using an online classification algorithm, allowing brain activity modulation [5].
There are two approaches based on the aim of the BCI application:
- Assistive BCI systems that specifically activate paralyzed muscles to ensure assistance in activities of daily living;
- Restorative BCI systems selectively induce use-dependent neuroplasticity to facilitate motor recovery [1].
Some companies make a great difference on the market by developing and selling exoskeletons for individual and independent use (as illustrated in Figure 4) and not only for medical centers and research, which makes a significant difference in stroke survivors’ daily lives.
Conclusions | Robotic-aided therapy in motor recovery after stroke
- Stroke is the leading cause of long-term disability, with limitations in daily life activities and life quality, but motor recovery is still possible after a stroke through exercise and therapy;
- There are emerging technologies, together with human-machine interfaces, used for assistance in neurorehabilitation and motor recovery that offer great support in patient’s ADLs;
- Robotic-aided therapy has been observed to be more effective compared to traditional physical therapy due to higher exercise intensity, higher movement controllability, and measurement reliability;
- The independence gained through robotic exoskeleton use provides patients with significant improvement in the quality of life and improved function of internal organs as well [5];
- Multiple types of interfaces are being developed and tested to trigger the assistance of the exoskeleton and better suit the level of assistance each user needs.
- Suppose exoskeletons were initially developed for professional medical personnel’s use only and are exclusively present in medical centers. In that case, nowadays, more and more companies are making this type of robotic aid available for private, personal use, thus making a huge difference in stroke survivors’ lives.
For more information on neurorehabilitation, visit:
- What is the impact of early life on brain and cognitive reserve?
- Does exercise induce neuroplasticity?
- Efficacy of placebo in managing pain for neurological disorders
We kindly invite you to browse our Interview category: https://efnr.org/category/interviews/. You will find informative discussions with renowned specialists in the field of neurorehabilitation.
References
- Frisoli, A; Solazzi, M.; Loconsle, C; Barsotti, M. New generation emerging technologies for neurorehabilitation and motor assistance. Acta Myol. 2016;35(3):141-144. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5416742/
- Gorgey, AS. Exoskeletons in rehabilitation World. J Orthop 2018, doi: 10.5312/wjo.v9.i9.112. Available from: https://pubmed.ncbi.nlm.nih.gov/30254967/
- TECTALES, An exoskeleton allows a tetraplegic patient to move, https://tectales.com/bionics-robotics/an-exoskeleton-allows-a-tetraplegic-patient-to-move.htm, 10.10.2019l
- Artemiadis P. EMG-based Robot Control Interfaces: Past, Present and Future. Adv Robot Autom 2012, 1:e107. doi:10.4172/2168-9695.1000e107. Available from: https://www.hilarispublisher.com/open-access/emg-based-robot-control-interfaces-past-present-and-future-2168-9695.1000e107.pdf
- Louis Korczowski PhD, Clinatec: Walking Again With a Brain-Computer Interface, https://louis-korczowski.org/clinatec-walking-again-with-a-brain-computer-interface