Rehabilitation of non-fluent aphasia patients

Author: Livia Popa, Oana Vanta
Keywords: non-fluent aphasia, post-stroke, computer-based therapy, Rehabilitation Gaming System, randomized controlled trial, RGS
Rehabilitation of non-fluent aphasia patients
Patients surviving a stroke or head trauma may still grapple with the brain injury’s fallout long after the event. For one, they may struggle to re-engage in seemingly basic tasks previously taken for granted, such as spoken communication. In medicine, loss of speaking ability, partial or complete, is called aphasia, an ancient word that means without (from the prefix a-) speech (from the word root -phasia) [1].
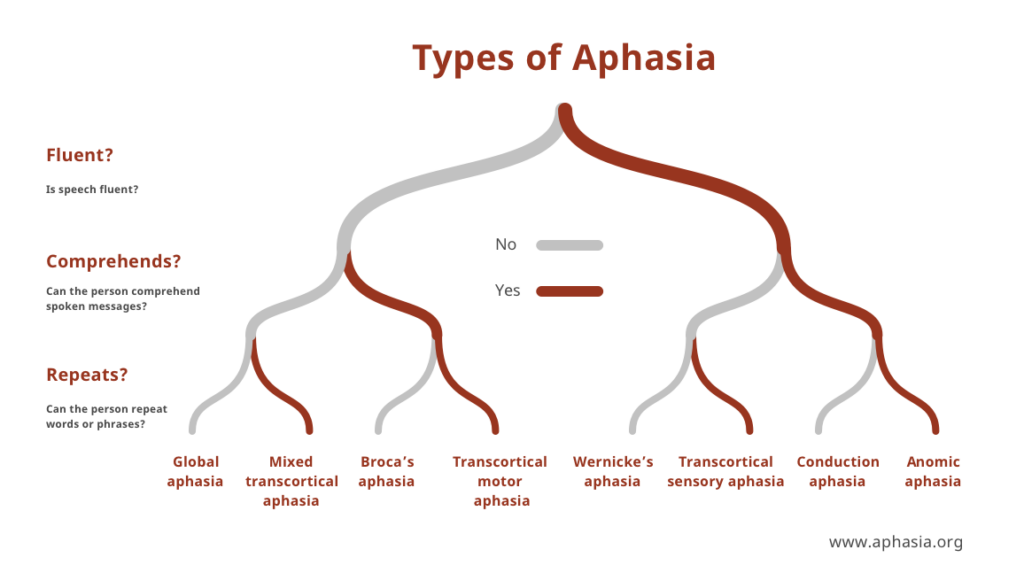
The spectrum of speech impediments labeled aphasia is particularly wide depending on what area(s) of the brain get damaged and how each is involved in the process of effective, meaningful communication.
Likewise, aphasia should be distinguished from dysarthria, a neurological problem that results in an inability to control the muscles used in speech and, consequently, in articulating words. Due to brain lesions in different areas, one patient may be physically unable to exercise the fine muscle control to utter their otherwise coherent reply to an interlocutor’s elicitation (dysarthria), and another may be incapable of finding the appropriate words (motor or non-fluent aphasia).
At the same time, another may respond with a flurry of perfectly pronounced but completely irrelevant “salad” of words (receptive, sensory, or fluent aphasia). However, another patient who can speak correctly and coherently may weirdly fail to repeat back what is said (conduction aphasia) or to describe what they are seeing (Figure 1). Of course, all such manifestations may be more or less severe based on the precise location and extent of the lesion(s) [1].
It is essential to acknowledge that someone suffering from non-fluent aphasia may not have a problem understanding what is being said and that they may also have the full cognitive ability to formulate their desired response in their mind. As such, and unlike other types of aphasia, the affected individual is likely to experience a build-up of frustration as they try to express themselves verbally [1].
Indeed, beyond the immediate toll of communication breakdown, people with aphasia are vulnerable to depression and social isolation, and their quality of life tends to deteriorate substantially. This has been established knowledge for at least a decade, as British researcher Hilari and her colleagues concluded in their systematic review from 2012. Their analysis of fourteen studies from all over the world revealed that communicative limitations and the severity of the aphasia were among the most important factors undermining the health-related quality of life for people with post-stroke aphasia [3].
Treatment options for non-fluent aphasia
The human body, including the brain, has an amazing capacity to heal itself. While this differs from one individual and age to another, one can expect that surviving a stroke will be followed by some degree of spontaneous, natural recovery. However, the language gets forgotten if not used even in normal circumstances, and guided neurolinguistic practice can go a long way towards getting the brain back in shape [3].
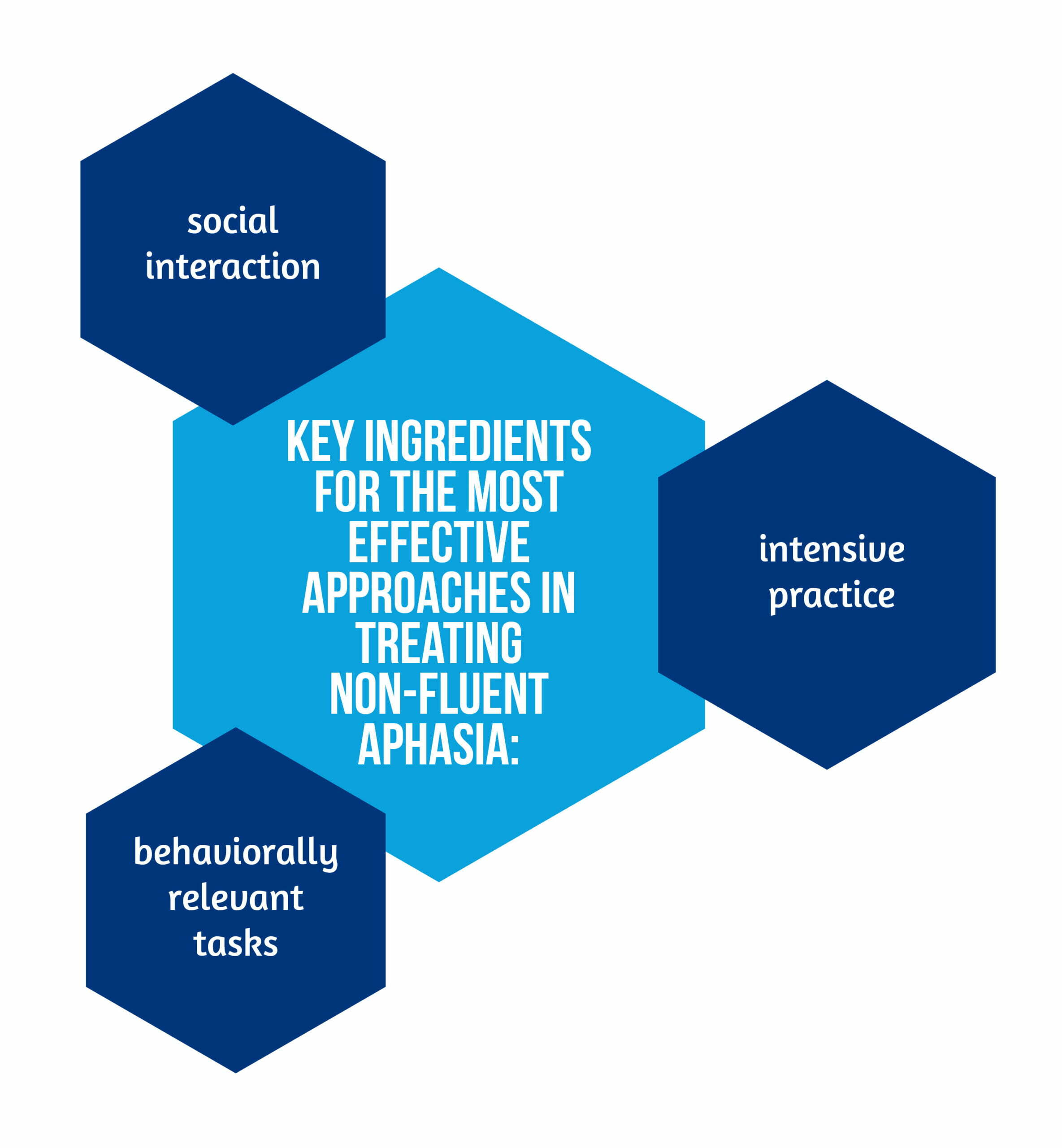
Clinical research into experimental post-stroke rehabilitation programs suggests that the most effective approaches for treating non-fluent aphasia have the key ingredients presented in the Figure 2 [4].
Unfortunately, scaling up such programs can get very expensive or may not be enough of a priority for healthcare systems worldwide. However, the advance and mainstreaming of digital technologies have prompted researchers to consider computer-based methods. Could they work as or more effectively but with fewer costs, especially when treating patients with persistent manifestations?
When it comes to the recovery of language and communication abilities after a stroke, either approach – conventional or innovative – is better than none. This was clearly shown by an Australian team who, in 2017, systematically reviewed the scientific literature to compare clinician-delivered and computer-based approaches to each other and the absence of intervention. At that time, research on computer-based applications for treating speech disorders was promising but still limited, so the authors concluded their review with an open invitation to fellow researchers to explore this potential [5].
Virtual reality gaming inspires experimental rehabilitation research
In 2019, the leading scientific journal Stroke published the results of a trial by a team of Spanish and German researchers who had developed a virtual reality-based therapeutic approach for treating non-fluent aphasia. Their experiment aimed to assess the effectiveness of computer-based language training built on the same three principles that work well in traditional settings – interactivity, intensiveness, and relevance [2]. The authors labeled it a Rehabilitation Gaming System (RGS) and based it on the RGS previously described by another group of researchers in 2010 in the Journal of Neuro-Engineering and Rehabilitation [6].
Grechuta and her colleagues designed their study to be as objective as possible. Seventeen consenting patients (nine men and eight women aged 34 to 68) were evaluated by speech and physical rehabilitation specialists specially trained to avoid bias. The patients were randomly assigned to either a control or an experimental group using a computer algorithm intended to make the two groups as homogenous as possible. Then, the eight patients in the control group benefited from standard treatment, while the other nine participated in the experimental RGS sessions. All the proceedings were carefully monitored, and several rounds of evaluations were organized [2].
All the participating patients had suffered a single stroke event 6 months to 12 years before, resulting in damage to left-hemisphere cortical areas (frontal, temporal, and parietal lobes) visible on MRI and CT scans. The non-fluent aphasia was moderate to severe in all the cases and was also persistent. None of the patients had cognitive disorders or motor impairments that might have influenced their performance or results [2].
The RGS sessions were conducted over eight weeks, during which all the patients were assessed multiple times – at the start, during, and at the end of the experiment. Both standard and RGS sessions were scheduled to last 30-40 minutes, 5 times per week, and the content of the materials was essentially the same. Moreover, follow-up data was collected after another eight-week period, during which the patients were instructed not to get more treatment elsewhere to allow researchers to measure and compare the stability of the outcomes [2].
The Rehabilitation Gaming System
The experimental RGS sessions took place according to an intensive language training protocol involving the interaction between two patients via digital avatars seen on each other’s computer screens. The avatars replicated the patients’ actual arm movements tracked and mapped digitally to enable them to handle virtual items. These were 3D representations of various objects, plants, and animals, such as bee, peach, ladder. For the standard therapy group, the images were printed on cards [2].
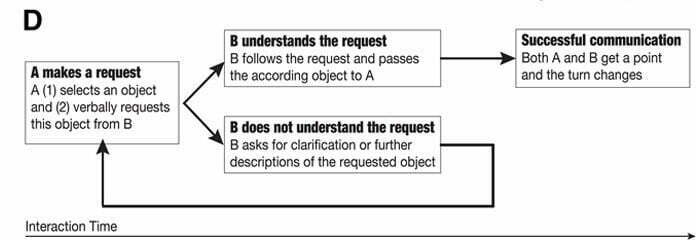
The session and game would start with one patient requesting an item by identifying it on their screen and then verbally asking the other patient for it. At any given time, three items would be visible for selection. If the request were expressed clearly enough for the second patient to understand, he/she would know what item to “give” by holding their hand over it for 3 seconds. If not, the second patient would need to ask for a verbal description or clarification. The successful hand-over of an item would result in both players scoring a point, and the game would continue in the same way by alternating turns until the collection of 36 points or the end of the session (see Figure 3) [2].
The results of the RGS experiment
The focus of the experiment was to assess the patients’ language function over time. For this, the research team used Boston Diagnostic Aphasia Examination subtests relevant to spoken communication, involving expression and comprehension. The results revealed significant improvements in linguistic performance at the 8-week and 16-week marks compared to the start for both the experimental and control groups. Although on average, the patients from the experimental group scored higher, the differences between the groups were not statistically significant, suggesting that either approach was beneficial [2].
In addition, the patients’ progress with uttering the vocabulary used in the sessions was evaluated repeatedly during the 8-week therapy period and after another 8 weeks of no intervention. Once again, significant improvements were recorded overall and in both groups. Interestingly, the patients who had participated in the experimental RGS sessions scored significantly better a month into the program.
Given that the experimental game procedure had included arm movements, the motor function of the patients’ hemiplegic right arms was assessed using the Fugl-Meyer Upper Extremity Scale. The results showed significant positive effects over time and significant differences in favor of the experimental approach.
A final set of interesting results from the therapy sessions regarded the interaction times, such as how long it took a pair of patients to select and collect an item correctly. All the patients who had played the experimental virtual reality game got gradually faster. Also, improved proficiency correlated significantly with vocabulary test scores in the experimental group.
Importantly, the patients’ communicative abilities outside the therapy sessions were also studied using a questionnaire called the Communicative Activity Log. This enabled the researchers to learn about the patients’ regular interaction patterns throughout the studied period. For example, the patients had to rate the frequency with which they had communicated with friends or strangers, on the phone, under stress, to ask or answer questions. Nevertheless, the collected data showed that both groups improved significantly over time, and although patients from the experimental group reported more frequent interactions, the differences between the groups were not statistically significant [2].
Conclusions
In conclusion, any therapy is better than none, and augmented is better than standard. Grechuta’s experiment from 2019 [2] shows how both standard and computer-based therapeutic approaches can benefit patients with non-fluent aphasia even when a substantial amount of time has passed since the stroke event. Isolating and measuring the differences between conventional methods and new ideas building on technology advancements is very hard to do, so the conclusions and recommendations should be taken with a grain of salt. The trial results indicate that an augmented, virtual reality, game-inspired rehabilitation approach can lead to better, more stable improvements of the lexical and motor skills directly targeted by the therapeutic tasks.
Now more than ever, this represents a promising direction for further research and meaningful clinical applications. In the aftermath of the Covid-19 pandemic, digital technology has become ubiquitous, and people from all walks of life are getting used to online interaction, compensating for any amount or reason for physical distance. High-performance augmented/virtual reality accessories and software integrations are being developed quickly. In this new context, people with aphasia should begin to have better access to better therapies.
For more information regarding post-stroke language impairment, visit:
- Naming therapy in patients with post-stroke aphasia
- Post-stroke language impairments treatment using tDCS (Transcranial direct current stimulation)
- Shedding light on Speech-Language Therapy: How stroke survivors can benefit from intensive rehabilitation training for chronic aphasia
References
- https://www.aphasia.org/aphasia-definitions/
- Grechuta K, Rubio Ballester B, Espín Munne R, Usabiaga Bernal T, et al. Augmented Dyadic Therapy Boosts Recovery of Language Function in Patients With Nonfluent Aphasia. Stroke 2019; 50(5):1270-1274; doi: 10.1161/STROKEAHA.118.023729
- Hilari K, Needle JJ, Harrison KL. What are the important factors in health-related quality of life for people with aphasia? A systematic review. Arch Phys Med Rehabil 2012; 93(1 suppl): S86–S95; doi: 10.1016/j.apmr.2011.05.028
- Berthier ML, Pulvermüller F. Neuroscience insights improve neurorehabilitation of poststroke aphasia. Nat Rev Neurol. 2011; 7:86–97. doi: 10.1038/nrneurol.2010.201
- Zheng C, Lynch L, Taylor N. Effect of computer therapy in aphasia: a systematic review. Aphasiology 2016; 30:211–244; doi: 10.1080/02687038.2014.996521
- Cameirão MS, Badia SBI, Oller ED, Verschure PFMJ. Neurorehabilitation using the virtual reality-based Rehabilitation Gaming System: methodology, design, psychometrics, usability and validation. J Neuroeng Rehabil 2010; 7:48; doi: 10.1186/1743-0003-7-48









