Post-stroke upper limb deficits – The EXPLICIT Trial

Authors: Victor Dabala, Oana Vanta
Keywords: stroke, upper limb, recovery, CIMT, EMG-NMS
Post-stroke upper limb deficits & rehabilitation – A convoluted evolution
As stroke is one of the most prevalent disorders, the same can be considered for upper limb (UL) impairment. With almost 75% of patients presenting with a level of arm dysfunctionality, UL disability can be considered the post-stroke complication with the highest incidence [1, 2].
The mechanisms that generate the favorable outcome of the arm recovery and the pathophysiology behind the installation of the functional loss are not entirely understood despite the ever-growing number of validated rehabilitation models, the absence of a clear path for approximating the evolution of UL disability, paired with the severity of the functional impact condition, and the persistence of upper limb impairment as a severe burden.
A critical period in the evolution of upper limb impairment is encompassed around the first 5 weeks after the onset of the event, with several scientific works strengthening the assumption. Therefore, a suitable example of an indicator of recovery is voluntary finger extension (FE), appearing mainly in the first 3 days after the acute event. Positive signs for FE are considered significant in the context of regaining a higher level of dexterity at a faster rate [1–3].
The Predict Recovery Potential (PREP) algorithm, a clinical tool combining different markers of rehabilitation (clinical, imaging, and neuropsychological), was involved in previous trials to predict upper limb functional evolution. The SAFE score (part of the PREP algorithm) calculates the rate of both shoulder abduction and finger extension, selecting the candidates from the stroke population that could benefit from the complete restitution of the UL deficit [4, 5].
The entire rehabilitation model discussed in the EXPLICIT trial is influenced by the grading of the FE level, generating two types of prognoses (favorable vs. unfavorable) [1].
For more insight into neurorehabilitation, visit:
- Obesity role in stroke prognosis and rehabilitation
- Rehabilitation of non-fluent aphasia patients
- SENSe: Assessing neurorehabilitation’s impact on the somatosensory function in stroke patients
The EXPLICIT Trial – Integration of Far-Out Therapies
The 2016 multi-center Randomized Clinical Trial (RCT) by Kwakkel et al. (EXPLICIT – EXplaining PLastICITy after stroke) involved 159 stroke survivors with upper limb impairment, divided into two groups. The criteria for allocating the patients to one of the two groups was the presence (or absence) of a finger extension range over 10 degrees – including the thumb and two or more additional fingers [1].
The trial’s main objective was the assessment of modified constraint-induced movement therapy (mCIMT) regarding the method’s efficiency in restoring UL functionality for a period of 24 weeks in patients with voluntary FE. The authors hypothesized that the administration of mCIMT daily for 3 weeks, compared to usual care alone, would produce a meaningful improvement in Action Research Arm Test (ARAT) values. The second pursued outcome was evaluating the efficiency of a different far-out therapy (electromyography-triggered neuromuscular stimulation or EMG-NMS) in the recovery of patients without voluntary finger extension, starting two weeks after stroke onset [1].
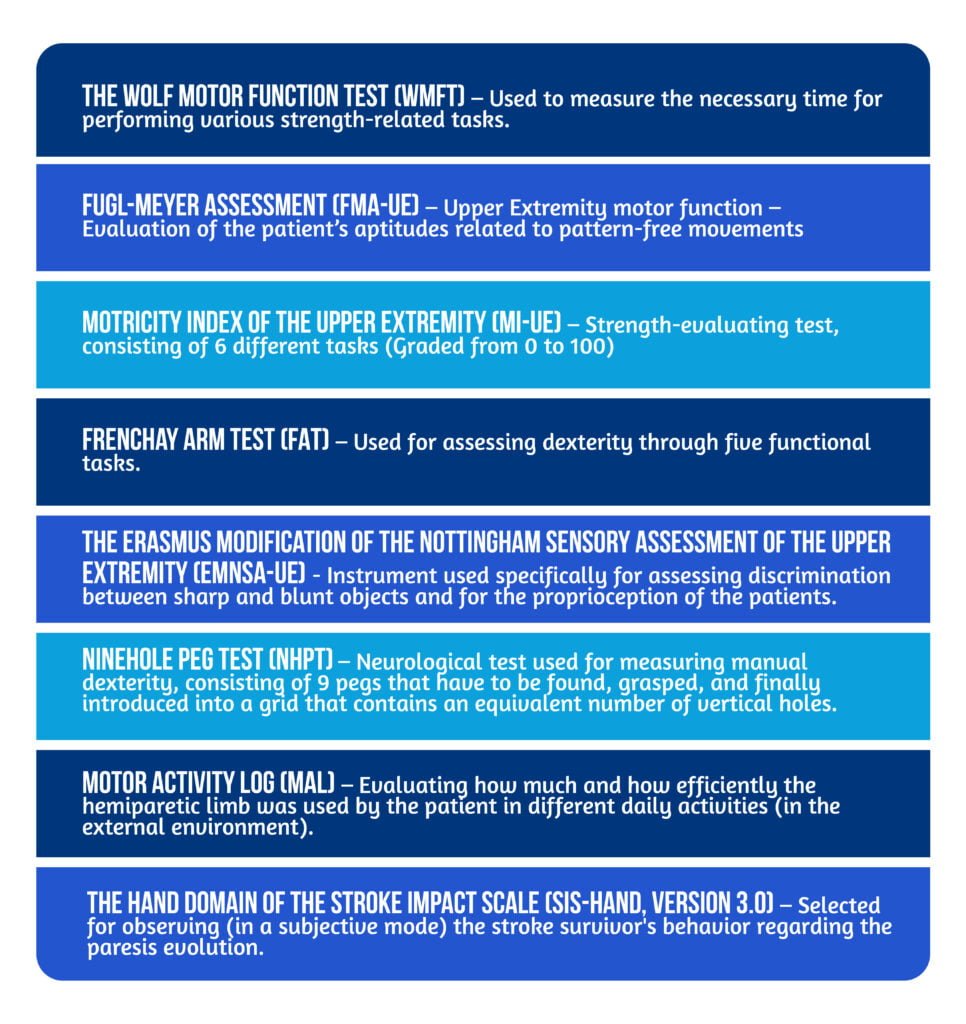
Therefore, 58 patients with a favorable outcome were part of a group that received mCIMT or usual care. In comparison, 101 patients with an unfavorable prognosis were allocated to a different group for which EMG-NMS was the standard therapy – compared to classical recovery. The patients were assessed for six months, starting 14 days after stroke onset, using the ARAT for the first five weeks and during the 8th, 12th, and 26th weeks. In addition to ARAT, several other clinical instruments were selected to assess arm motricity [Tabel 1] [1, 6].
In a trial by Dromerick et al., the results of constrained-induced movement therapy were contradictory, with 1 to 2 hours per day of CIIMT not considered superior to standard recovery models. Moreover, daily three-hour sessions negatively impacted functional improvement [6].
Electromyography-triggered neuromuscular stimulation is considered promising, especially after a period of time since the event (e.g., subacute to chronic strokes). The mechanisms behind EMG-NMS could consist of shifts in overall cortical activity and in terms of the excitability level of the stroke survivor. An essential aspect of EMG-NMS is the lack of scientific data regarding its efficiency in the acute-early subacute stages of stroke in patients without voluntary FE [7, 8].
The EXPLICIT trial was an observer-blind trial, with patients being stratified according to the grading of finger extension in the first two weeks after stroke, followed by a randomizing process regarding the association of the experimental or standard therapy. The personnel computing the randomizing procedure were not part of creating the treatment protocol [1].

Different Interventions for Each Individual Group
The intervention differed in relation to the assessed population. The mCIMT group performed various tasks-related actions that required using the paretic arm, especially movements in which the patients used their finger extensors. For the entire session of 60 minutes (administrated as a single session or equally divided into two 30-minute ones), the stroke survivors used a padded mitt. The mitt was also used for three more hours each day, for 3 consecutive weeks, and a total of 5 weeks after the acute neurological event [1].
Regarding the patients that underwent EMG-NMS therapy, two thirty minutes sessions of electrical stimulation (of the fingers’ extensors muscles) were applied daily. A Stilwell-Med4 system was used during the procedures (Ottobock Healthcare Products GmbH, Vienna, Austria) [1, 6, 9].
For a complete therapeutical effect, active movements from patients had to be performed (e.g., the dorsiflexion of the wrist). If the EMG device recorded no activity of the hemiparetic limb, patients were instructed to concomitantly abduct the impaired arm for the generation of an electrical response (the so-called Soques phenomenon – elevation of the impaired arm causes the paralyzed fingers to extend concomitantly). Five seconds of stimulation were followed by 25 seconds of rest. For facilitating a response, a virtually-generated game was used as a form of visual feedback (As a hot air balloon that had to be raised over a mountain – in relationship with the degree of FE) [1].
The primary outcome for both recovery models was the ARAT score, a neurological instrument used for evaluating the functional reserve of the patient regarding comprehension of, moving, or releasing various objects. A specifically adapted version was used (applying 15 out of the 19 original test items) [1, 3].
The Results – Disentangling One Model from Another
The superiority of modified constraint-induced movement therapy compared to standard care in the favorable prognosis group – At five, eight, and twelve weeks after the acute onset of the ischemic stroke (with a significant difference – 6, 7, and respectively 7 points increases in the ARAT score each week).
No significant data that could favor the beneficial effect of electromyography-triggered neuromuscular stimulation against standard recovery measures were founded.
Of all the secondary outcome instruments, only the SIS-Hand (at eight weeks post-stoke) was considered statistically relevant in relation to the favorable outcome group (in favor of mCIMT) [1].
Consolidating the Role of Finger Extension
Two important aspects define the EXPLICIT trial; up front, It is the first trial that tested the capability of the range of finger extension in predicting upper limb function recovery, enriching the previous evidence regarding the role of FE in the domain of rehabilitation (e.g., the PREP algorithm). Furthermore, it implied the use of both CIMT and EMG-NMS, considered far-out therapies by some specialists, therefore improving the clinical data regarding their role and efficiency. Considering the topics above, the Kwakkel et al. trial could be considered a pioneer in properly integrating and assessing novel upper limb recovery measures.
As the rehabilitation field is on a constant journey to find valuable information regarding innovative therapies and models, upper-limb management in stroke patients remains a hard-to-bear challenge, in contrast to the vast array of interventions available. Scientific works like the EXPLICIT trial set the context for creating novel pathways regarding favorable outcomes in stroke populations, encouraging the possibility of drastically reducing the burden created by post-stroke deficits.
References
- Kwakkel G, Winters C, van Wegen EE, Nijland RH et al. Effects of Unilateral Upper Limb Training in Two Distinct Prognostic Groups Early After Stroke: The EXPLICIT-Stroke Randomized Clinical Trial. Neurorehabil Neural Repair. 2016;30(9):804-16. doi: 10.1177/1545968315624784.
- Teasell R, Salbach NM, Foley N, Mountain A, et al. Canadian Stroke Best Practice Recommendations: Rehabilitation, Recovery, and Community Participation following Stroke. Part One: Rehabilitation and Recovery Following Stroke; 6th Edition Update 2019. Int J Stroke. 2020;15(7):763-788. doi: 10.1177/1747493019897843.
- Kwakkel G, Kollen BJ, Van der Grond J, Prevo AJ. Probability of regaining dexterity in the flaccid upper limb: impact of severity of paresis and time since onset in acute stroke. Stroke. 2003;34:2181-2186. DOI: 10.1161/01.STR.0000087172.16305.CD
- Stinear CM et al. The PREP algorithm predicts the potential for upper limb recovery after stroke, Brain, 2012, 135:2527-2535. DOI: 10.1093/brain/aws146
- Stinear CM et al. PREP2: A biomarker-based algorithm for predicting upper limb function after stroke, Annals of Clinical and Translational Neurology, 2017, 4(11): 811–820. DOI: 10.1002/acn3.488
- Dromerick AW, Lang CE, Birkenmeier RL, et al. Very Early Constraint-Induced Movement during Stroke Rehabilitation (VECTORS): a single-center RCT. Neurology. 2009;73:195- 201. doi: 10.1212/WNL.0b013e3181ab2b27
- Francisco G, Chae J, Chawla H, et al. Electromyogram-triggered neuromuscular stimulation for improving the arm function of acute stroke survivors: a randomized pilot study. Arch Phys Med Rehabil. 1998;79:570-575. DOI: 10.1016/s0003-9993(98)90074-0
- De Kroon JR, IJzerman MJ, Lankhorst GJ, Zilvold G. Electrical stimulation of the upper limb in stroke: stimulation of the extensors of the hand vs. alternate stimulation of flexors and extensors. Am J Phys Med Rehabil. 2004;83:592-600. DOI: 10.1097/01.phm.0000133435.61610.55
- Gladstone DJ, Danells CJ, Black SE. The fugl-meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil Neural Repair. 2002;16(3):232-40. doi: 10.1177/154596802401105171.









