Pregnancy and stroke: What are the risks and implications?

Author: Livia Popa, Oana Vanta
Keywords: pregnancy, stroke, risk factors
Pregnancy and stroke | what kinds of strokes can occur during pregnancy?
To appreciate the significance of a stroke during pregnancy, it is important first to clarify what we generally call a stroke. The word refers to different cerebrovascular accidents or events, some ischemic and some hemorrhagic, both of which can occur during pregnancy. Each is briefly explained below and illustrated in Figure 1.
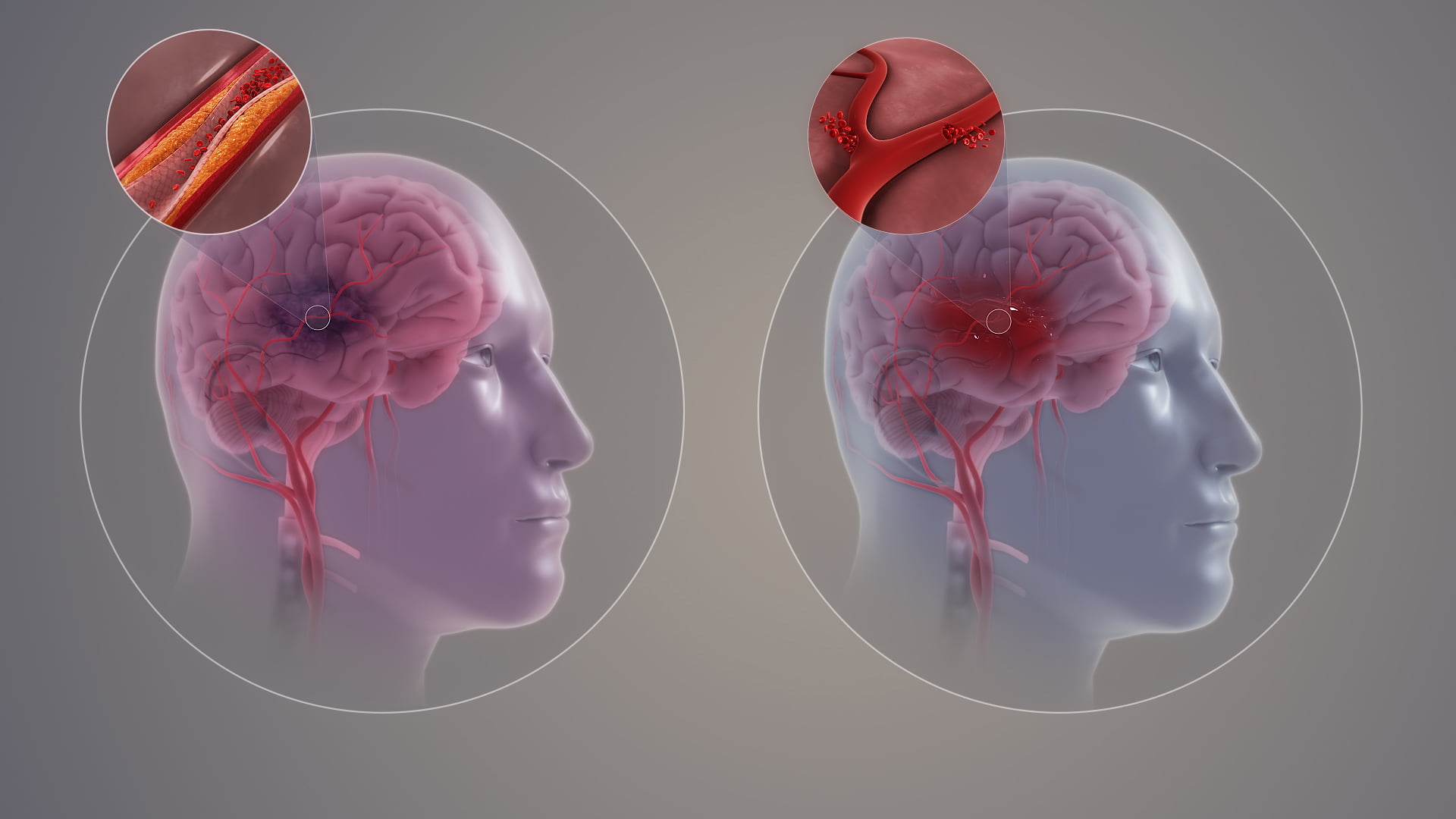
An ischemic stroke (IS) is when a blood vessel gets clogged and, as a result, the oxygen supply to a certain area or areas of the brain is cut off. Such blockage is typically caused by an obstructive blood clot or a condition called atherosclerosis, which is the slow buildup of plaque inside the blood vessel wall [2].
By contrast, a hemorrhagic stroke (HS) is when a blood vessel tears and causes bleeding inside the brain. Chronic hypertension is a common condition that can affect the integrity of a blood vessel wall and eventually lead to its rupture, especially where the wall is already weakened or bulging outward due to an existing malformation or an aneurysm [2].
Both types of strokes are possible during pregnancy. The most frequent ones are hemorrhagic, although ischemic strokes are the most common in the general population. This is mainly because of pregnancy-related hypertension, a condition called preeclampsia [3].
Click here to learn more about the different stroke types and subtypes.
How common are strokes during pregnancy?
For a woman of childbearing age, the risk of having a stroke for the first time in her life is low. A systematic analysis of studies published between 1990 and 2017 found an incidence of 30 strokes in 100 000 pregnancies globally [4]. At a national level, for example, official Canadian records from 2003-2016 list no more than 524 stroke cases (most of which were hemorrhagic) in the context of almost 4 million deliveries. However, data from all over the world suggests that the incidence, even if small, is increasing [5].
What are the risk factors for stroke during pregnancy?
The risk of stroke may increase during pregnancy and in the postpartum period due to the factors listed in Table 1 below. These are grouped into pre-existing factors and those specifically related to the pregnancy.
| General maternal characteristics and medical conditions preceding the pregnancy | Medical conditions related to the pregnancy period |
|---|---|
| older age (35-39 and especially ≥40 years) | preeclampsia |
| race (African American and Asian) | eclampsia (hypertensive seizures/convulsions) |
| (congenital) heart disease | vessel wall defects |
| chronic hypertension | cerebral venous thrombosis |
| coagulation disorders (e.g., thrombophilia) | gestational diabetes |
| aneurysms and vascular malformations | cesarean delivery |
| diabetes mellitus | postpartum hemorrhage |
| rheumatological conditions | infections |
| sickle cell disease | |
| obesity | |
| HIV infection | |
| migraines | |
| smoking |
Can pregnancy cause a stroke?
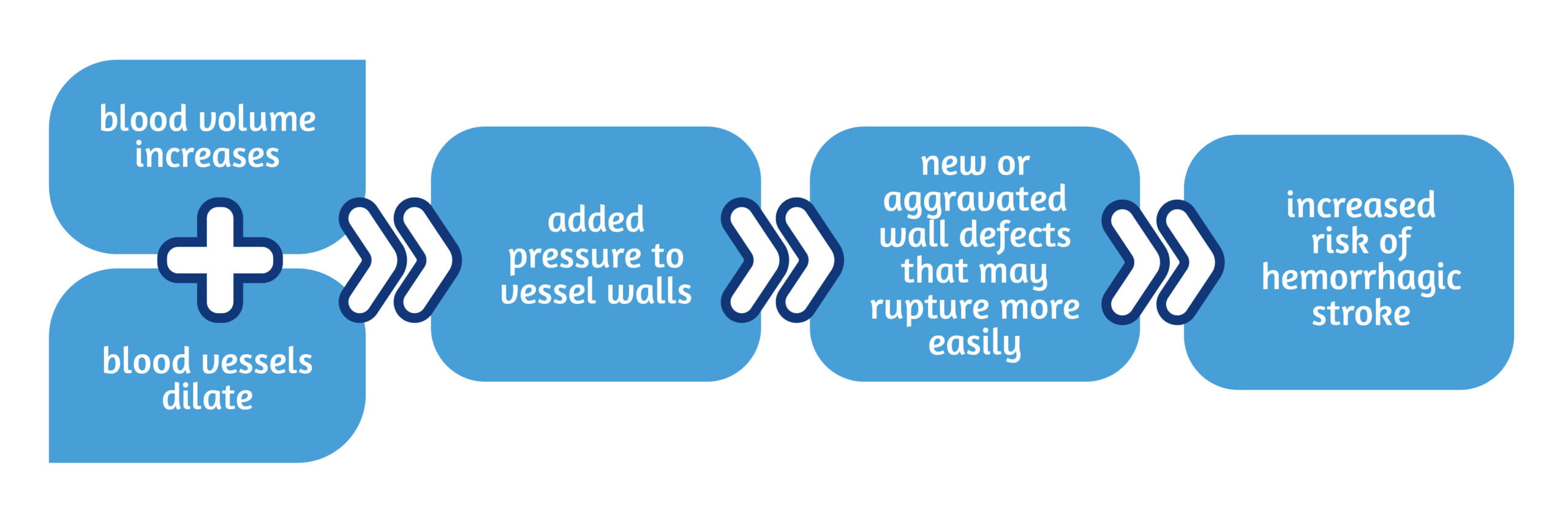
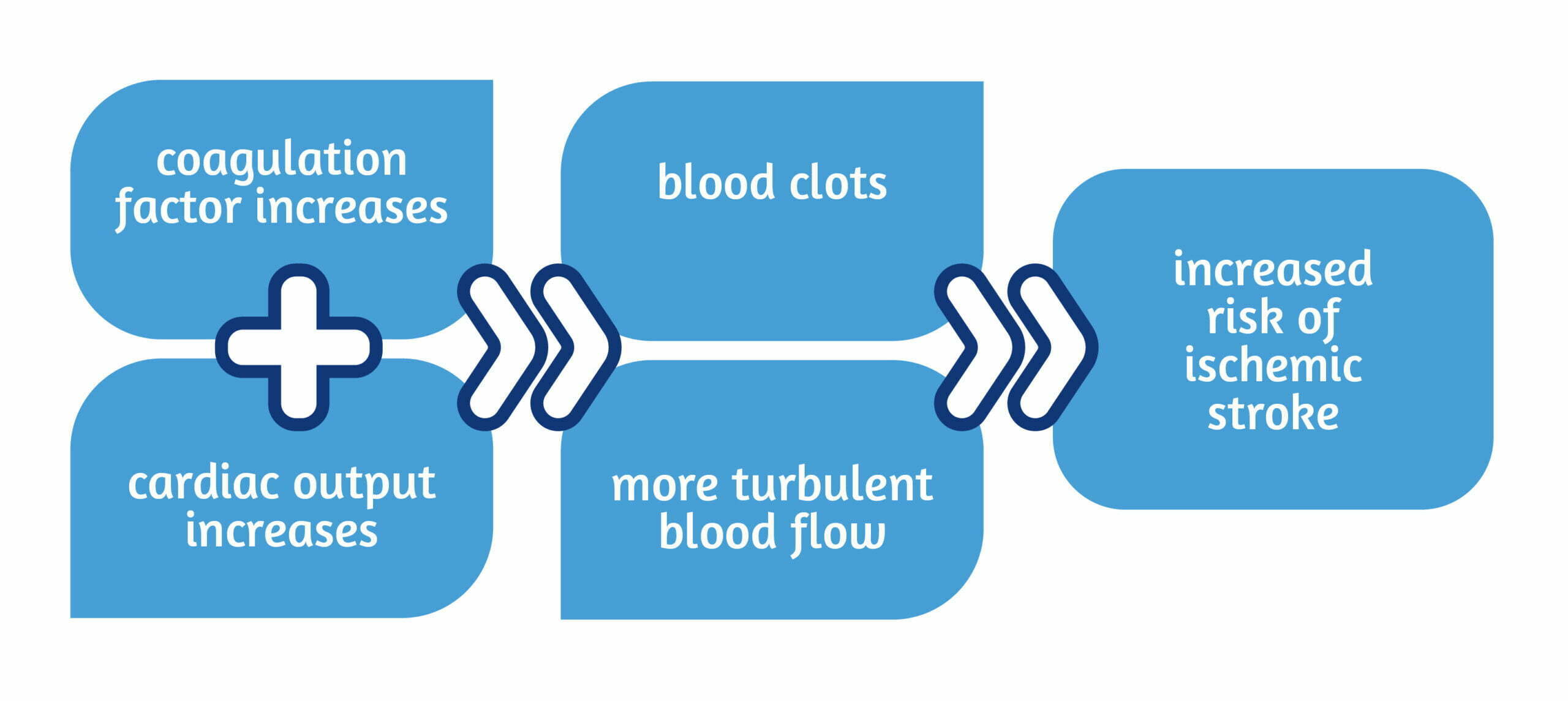
No, pregnancy per se does not cause a stroke. During pregnancy, the woman’s body undergoes profound changes necessary for the baby to develop and for birth. Some of these processes involve the cardiovascular system and may facilitate the conditions for ischemic or hemorrhagic stroke to occur, as illustrated in Figures 2 and 3 below:
Can stroke also occur soon after giving birth or even reoccur later in life?
Unfortunately, the answer is yes to both questions:
- A stroke can occur during the pregnancy and the postpartum period. The critical stages, especially for women diagnosed with preeclampsia, are the third trimester of pregnancy and the first 6 weeks after giving birth [3].
- For women with histories of stroke during pregnancy or the postpartum period, the risk of recurrence was found to be only 2%. Also, complications during additional pregnancies do not appear to be higher than reported generally [7, 8].
How dangerous is a stroke during pregnancy?
The short answer is very, with the first 24 hours being critical. The more rapid the intervention, the more the brain and its functions can be preserved [7].
- Stroke events are medical emergencies that can lead to significant disability; the main cause of long-term impairment after giving birth is stroke during pregnancy [5]. They are also life-threatening. According to official records of maternal deaths in the US during 2011-2014, stroke was the cause in 7.4% of cases [3]. The same result was found for maternal deaths in Canada during 2003-2016 [5].
- In the US, another 6.8% of maternal deaths were due to hypertension, which further highlights the importance of taking preeclampsia (pregnancy-related hypertension) seriously [3].
What are the symptoms of stroke during pregnancy?
Pregnant women who experience symptoms suggestive of a possible stroke should seek and receive urgent medical attention [6, 7]. These are highlighted in Figure 4.

Except for neck stiffness, which can be a sign of hemorrhagic stroke, ischemic and hemorrhagic strokes can trigger these symptoms. Because the two stroke types require different treatment approaches, accurate diagnosis is crucial [7].
What diagnostic investigations are safe during pregnancy to confirm a stroke?
To definitively diagnose stroke, an emergency head CT scan works best. The potential adverse effects of radiation on pregnant women and fetuses are minimal to negligible, while the stroke-associated risks are serious and impending. Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) can be effective diagnostic methods that avoid radiation. These investigations should best be carried out without the use of contrast agents. Ultrasonography may seem the safest, but it does not help diagnose strokes [6, 9, 10].
What are safe and effective treatments for stroke during pregnancy?
It is not entirely clear if therapies known to be safe and effective for the general population are equally so for pregnant women and their fetuses. This is because most clinical trials do not include pregnant women, considered a vulnerable group [6, 7].
- For acute ischemic strokes, the top priorities are to eliminate the blockage and restore blood flow. Available evidence suggests that therapies restoring blood flow, also called reperfusion therapies, can benefit pregnant and non-pregnant women similarly. While there can be consequences to administering thrombolytic agents to a pregnant woman, certain drugs contain big enough molecules that cannot cross the placenta and affect the fetus. Alternatively, it may be possible to remove blood clots mechanically using a procedure called thrombectomy [6, 7, 10, 11].
- For hemorrhagic strokes, the top priorities are to stop the bleeding, reduce intracranial pressure, repair the damaged vessel, and prevent further rupture. The management of ruptured aneurysms and vascular abnormalities is always surgical, and it requires detailed imaging. Depending on the exact location and extent of the damage, the intervention may be more or less invasive. The surgical interventions significantly reduced maternal and fetal mortality [6, 7].
Importantly, to prevent stroke during pregnancy from occurring, any hypertension and hypertensive seizures should be treated as aggressively as necessary [6]. Scientific evidence suggests that eliminating hypertension during pregnancy can reduce the incidence of related stroke cases by as much as 20% [5].
What does post-stroke rehabilitation involve for a pregnant female patient?
Beyond the initial treatment addressing the cause of the stroke event, the subsequent rehabilitation process is based on existing standards and practices for general post-stroke management. As in all stroke cases, the sooner the rehabilitation, the better the recovery. For pregnant patients, interdisciplinary communication and teamwork are essential to effectively consider and adapt to the particular needs of each such patient. Notably, the fetus will be monitored more frequently to check for any signs of compromised growth or well-being, and findings will inform delivery decisions [12].
Can a woman who had a stroke during pregnancy give birth naturally?
In theory, yes, but the decision to proceed with vaginal or cesarean delivery should be made on a case-by-case basis taking into consideration all the relevant factors, such as the woman’s blood coagulation factor, the precise impact of the stroke event on the brain, the presence of further risk factors. The same can be said about which type of pain management and anesthesia would bring the most benefits without additional risks [3].
How can stroke during pregnancy be prevented?
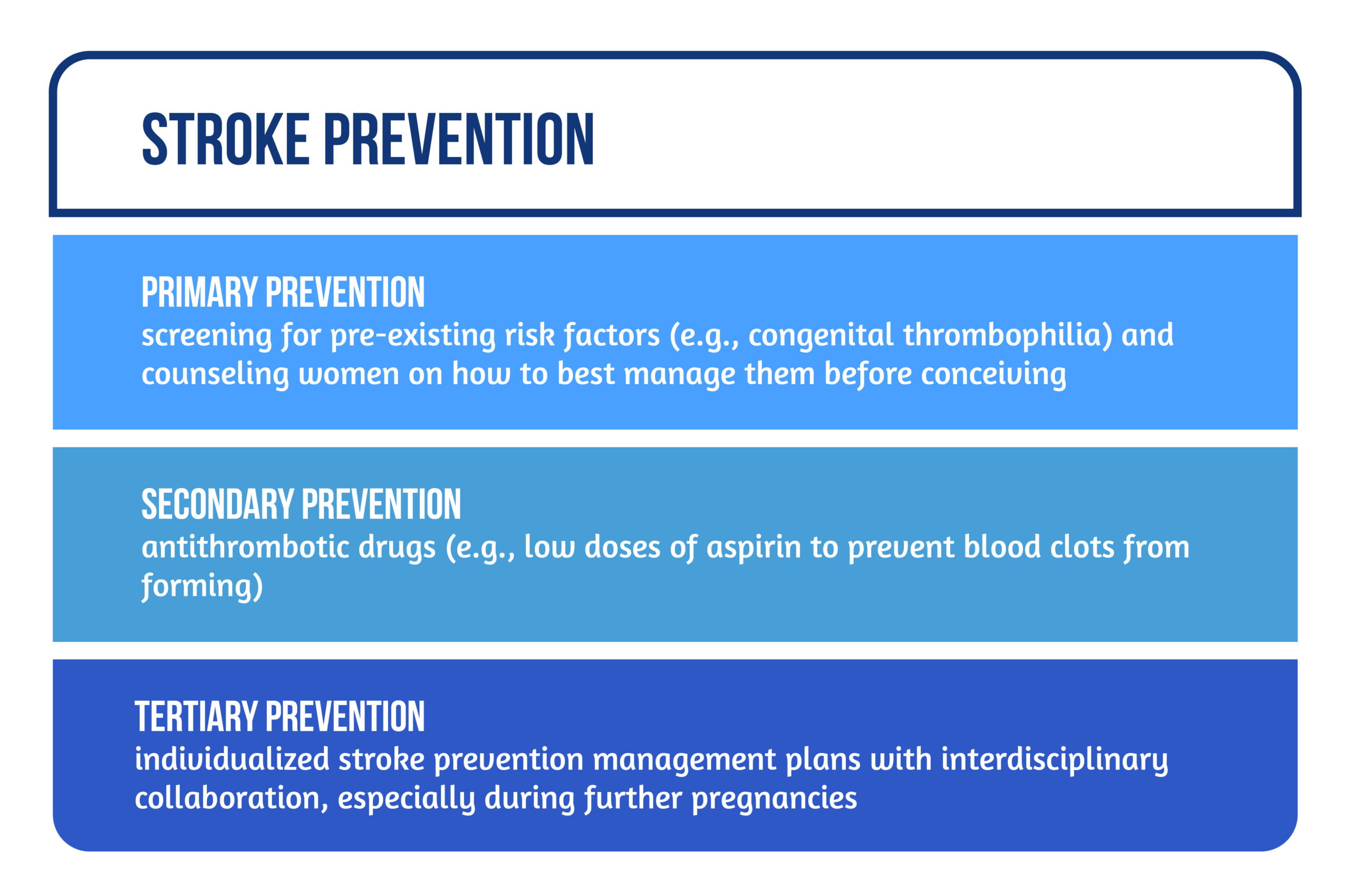
Stroke prevention works at different levels, as highlighted in Figure 5:
- Primary stroke prevention is about preventing a stroke from occurring in the first place – this can best be done by screening for pre-existing risk factors (e.g., congenital thrombophilia) and counseling women about how to best manage them before conceiving;
- secondary prevention is about early detection and intervention before a stroke event can take hold and incur any damage – in pregnant women at risk, this is usually achieved with antithrombotic drugs, such as prescribing low doses of aspirin to prevent blood clots from forming;
- tertiary prevention is about preventing another stroke at a later date – for women with a history of stroke, individualized stroke prevention management plans are necessary and require interdisciplinary collaboration, especially during further pregnancies [13].
What are some key points to remember?
All in all, women who are concerned about the risk of stroke during pregnancy should know that:
- a stroke is a medical emergency that can cause long-term disability or even death;
- pregnancy-related physiology can facilitate the conditions for stroke, but pregnancy does not cause stroke, and stroke events during pregnancy are rare;
- pregnancy-related hypertension, known as preeclampsia, is a significant risk factor that should be managed as aggressively as necessary;
- symptoms indicative of stroke include severe headache, altered consciousness, one-sided sensorial and/or motor impairment;
- accurate diagnosis with a CT scan or MRI is imperative, as ischemic and hemorrhagic strokes require different treatments;
- post-stroke management during pregnancy requires effective teamwork across medical disciplines and careful monitoring, including of the fetus;
- having a stroke during pregnancy does not necessarily limit a woman’s ability to give birth naturally or to bear more children in the future.
For more information about neurorehabilitation and stroke, visit:
- How did COVID-19 impact stroke rehabilitation?
- How can music improve stroke recovery?
- How does gender influence stroke and neurorehabilitation?
References
- https://commons.wikimedia.org/wiki/File:Types_of_Stroke.jpg
- American Stroke Association. Dallas: American Heart Association. Types of Stroke and Treatment; 2022; Available from: https://www.stroke.org/en/about-stroke/types-of-stroke
- Miller E, Leffert L. Stroke in Pregnancy: A Focused Update. Anesth Analg 2020; 130(4):1085-1096; doi:10.1213/ANE.0000000000004203
- Swartz RH, Cayley ML, Foley N, Ladhani NNN, et al. The incidence of pregnancy-related stroke: A systematic review and meta-analysis. Int J Stroke 2017; 12(7):687-697; doi: 10.1177/1747493017723271
- Liu S, Chan WS, Ray J, Kramer M, Joseph KS. Stroke and Cerebrovascular Disease in Pregnancy. Incidence, Temporal Trends, and Risk Factors. Stroke 2019; 50:13-20; doi: 10.1161/STROKEAHA.118.023118
- Sells CM, Feske SK. Stroke in Pregnancy. Semin Neurol 2017; 37(6):669-678; doi: 10.1055/s-0037-1608940
- Sanders BD, Davis MG, Holley SL, Phillippi JC. Pregnancy-Associated Stroke. J Midwifery Womens Health 2018; 63(1):23-32; doi: 10.1111/jmwh.12720
- Karjalainen L, Tikkanen M, Rantanen K, Laivuori H et al. Pregnancy-associated stroke – a systematic review of subsequent pregnancies and maternal health. BMC Pregnancy Childbirth 2019; 19(1):187; doi: 10.1186/s12884-019-2339-y
- Chansakul T, Young GS. Neuroimaging in Pregnant Women. Semin Neurol 2017; 37(6):712-723; doi: 10.1055/s-0037-1608939
- Treadwell SD, Thanvi B, Robinson TG. Stroke in pregnancy and the puerperium. Postgrad Med J 2008; 84(991):238-45; doi: 10.1136/pgmj.2007.066167
- Leffert LR, Clancy CR, Bateman BT, Cox M et al. Treatment patterns and short-term outcomes in ischemic stroke in pregnancy or postpartum period. Am J Obstet Gynecol 2016; 214(6):723.e1-723.e11; doi: 10.1016/j.ajog.2015.12.016
- Ladhani NNN, Swartz RH, Foley N, Nerenberg K et al. Canadian Stroke Best Practice Consensus Statement: Acute Stroke Management during pregnancy. International Journal of Stroke 2018; 13(7):743-758 ; doi:10.1177/1747493018786617
- Swartz RH, Ladhani NNN, Foley N, et al. Canadian stroke best practice consensus statement: Secondary stroke prevention during pregnancy. International Journal of Stroke 2018; 13(4):406-419; doi:10.1177/1747493017743801









