Efficacy of virtual reality augmented robot-assisted gait training in chronic stroke – results from a randomized controlled single-blind trial.

Authors: Irina Benedek, Oana Vanta
Keywords: Stroke, Virtual reality, Rehabilitation, Robot-assisted gait training
The impact of stroke
Stroke remains the leading cause of morbidity and disability worldwide, significantly impacting the quality of life. Sensor and motor difficulties in patients who suffered a cerebrovascular accident, such as loss of postural control, muscular weakness, alterations of muscle tone, and decreased cognitive skills, limit daily activities by impairing balance and walking.
Furthermore, stroke has a significant socioeconomic influence on society at a global level. In terms of media attention, patient and caregiver understanding, service advancements, and research, stroke is assuming a growing influence. Over 9 million stroke survivors make up the 4.5 million stroke fatalities annually. If they live to be 85 years old, roughly one in four males and nearly one in five women that age may anticipate having a stroke. [1–3].
Neurorehabilitation is mainly focused on the recovery processes in the acute and subacute (first 3 to 6 months) stages of stroke. Several benefits have also been observed in chronic patients (6 months post-stroke) [4]. Relearning motor skills and neuroplasticity are essential concepts when it comes to rehabilitation. Therefore, one of the aims of neurological recovery is to obtain the best results and translate the lessons into improving the patient’s everyday life.
To better undestand stroke and stroke neurorehabilitation, visit:
- Shedding light on Speech-Language Therapy: How stroke survivors can benefit from intensive rehabilitation training for chronic aphasia
- Interview with Prof. Natan Bornstein (Chair of Israeli Stroke Society)
- Interview with Prof. Marc Fisher (President of the World Stroke Organization)
Innovative technology-supported techniques for rehabilitation programs – Robotic and Virtual Reality (VR) devices
Due to their numerous benefits in managing stroke, technology-supported rehabilitation techniques like Virtual Reality (VR) and robot-assisted gait systems have recently been studied and used for this purpose. VR training has been demonstrated to:
- boost neuroplasticity
- improve movement quality
- and functional capacity in stroke patients [4].
While robot-assisted gait training (RAGT) has been proven to enhance gait and balance [5], using VR in conjunction with RAGT enables the sensory component of the nervous system to be included in rehabilitation programs. Furthermore, according to medical data, adding VR to robotic treatment helps stroke patients feel more motivated and actively participate in their recovery training [6].
The benefits of virtual reality-assisted neurorecovery programs
There are numerous VR applications in neurorehabilitation [7], as described in Figure 1 below:

Some studies reported that VR training, in addition to conventional therapy, was more effective on functional measures in patients with chronic stroke than conventional therapy alone. With a three-week course of VR combined treadmill training, Xiao et al. found an increase in activation of the primary sensorimotor cortex ipsilateral to the lesion and supplementary motor region bilaterally; an increase in gait speed was also noticed [7].
The primary goal of the study by Kayabinar and the team was to demonstrate the impact of a combined regimen of VR and RAGT on the ability of dual-task performance in chronic stroke patients. The secondary goal was to assess how VR training in conjunction with RAGT influenced chronic stroke patients’ gait, mobility, balance, fear of falling, and level of independence in daily activities [7].
Study addressability and parameters evaluation
Between February 2019 and June 2019, thirty chronic stroke patients took part in a randomized controlled single-blind trial at the inpatient rehabilitation center. They were randomly and equally assigned into two groups:
- virtual reality-augmented robot-assisted gait training (VR-RAGT) and
- control group robot-assisted gait training (RAGT) performed with RoboGait [7].
RoboGait was an exoskeleton gait robot. It included a knee and hip support that could be programmed to move a person’s lower extremities on a treadmill along a predetermined path. Overall, the technology included a treadmill, a dynamic body weight support system, and a motorized robotic orthosis that enabled patients to walk with a natural stride. The motorized gait orthosis was computer-controlled and made to facilitate joint mobility at different walking rates. In addition to RAGT, patients in the trial group engaged in two-dimensional VR gaming on the device’s 40-inch screen created by RoboGait. The patients were challenged to navigate a dense forest setting without colliding with any of the trees while attempting to gather the coins that showed on the screen, all while collecting points for the system. Moreover, both groups engaged in patient-specific neurodevelopmental therapy programs, including lower, upper, and trunk approaches based on their functional levels and requirements, in addition to the therapies [7].
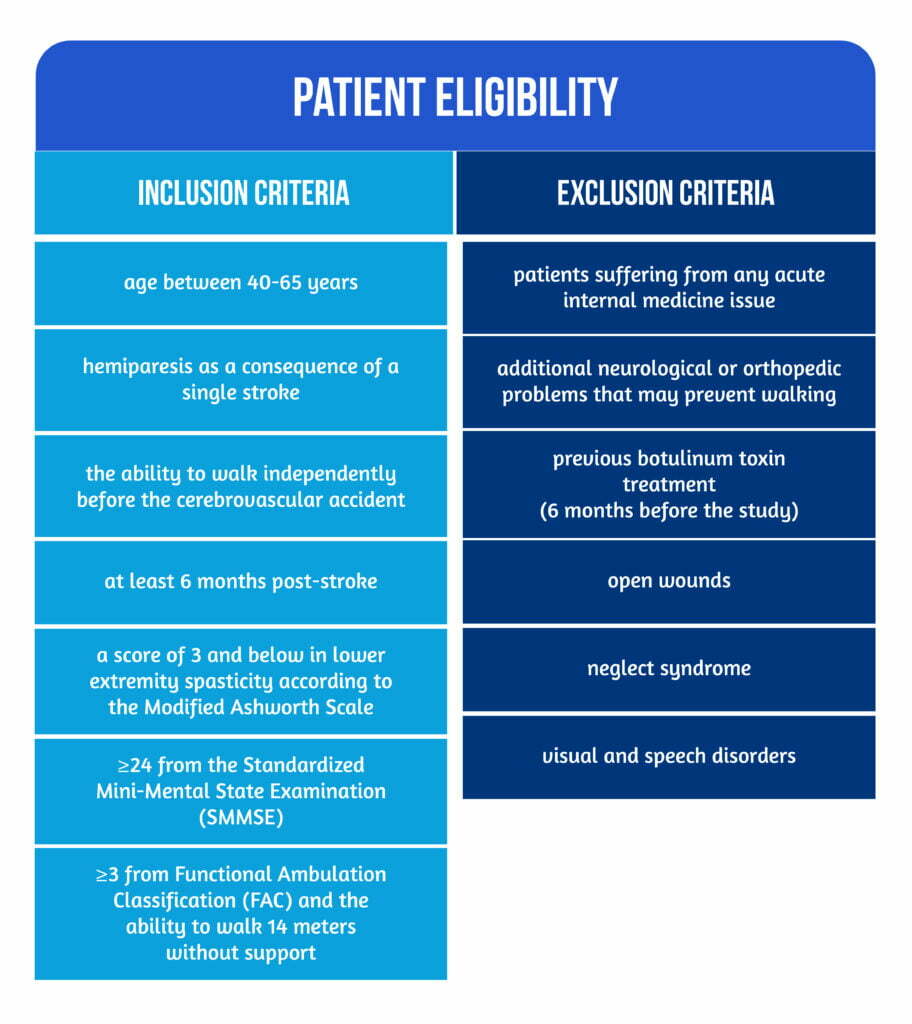
The patient eligibility criteria are mentioned in Figure 2 below:
There were two physiotherapists in the study: one responsible for randomization and treatment, and the other responsible for assessment to avoid bias.
The functional parameters used to quantify the results were applied at baseline and after 6 weeks of treatment, as represented in Table 1.
| Parameter | Scale/ Measurement tools | Evaluation/ Details |
| Cognitive function | Mini-Mental State Examination (MMSE) | Evaluates language, attention and calculation, recollection, orientation, and registration |
| Ambulation | The Functional Ambulation Classification (FAC) | Evaluates ambulation levels including six distinct functional categories, ranging from 0 (range 0- non-functional ambulation) to 5- FAC (ambulator-independent). |
| Dual-task performance | 10-Meter Walk Test (10MWT) | Using different motor and cognitive tasks in addition to the 10-Meter Walk Test (10MWT), which represented the primary motor task. Dual-task interference is the change in performance caused by engaging in two tasks at once. The amount of dual-task interference is evaluated by using the dual-task effect (DTE) formula evaluated the amount of dual-task interference. DTE is calculated by comparing the results of the two tasks individually and jointly (DTE = dual-task performance – single-task performance). |
| Gait | The Functional Gait Assessment (FGA) | Evaluating the patients’ gait characteristics under various circumstances ( e.g., walking normally, walking at varying speeds, turning one’s head to the left and right while walking, walking on one’s heels, and climbing stairs ). |
| Mobility | Rivermead Mobility Index | Reliable for stroke patients and assesses functional mobility in various activities, from turning over in bed to jogging. |
| Balance | The Berg Balance Scale (BBS) | Evaluation of balance while performing different functional tasks |
| Fear of falling | The Fall Efficacy Scale International (FES-I) | |
| Daily life activities | Functional Independence Measure | Independence in daily tasks |
Table 1. Functional parameters and their usage [7-9]
Results, Discussion & Study limitations
In the study by Kaybinar et al., both groups underwent a non-progressive gait training program at a standard pace and with weight support. The study was a randomized, controlled, single-blind trial that examined the effects of VR-augmented RAGT on dual-task performance and functional measurements in chronic stroke patients. The findings showed that the impact of VR-augmented RAGT on the above-mentioned functional parameters was comparable to those of RAGT-only approaches [7].
After treatment, the study group’s performance on dual tasks and gait speed showed a substantial change, but there was no difference between the study and control groups. The control group, which had superior scores from baseline measures, showed no change following the therapy, according to the data. However, the research group with lower beginning performance ratings demonstrated considerable gains.
It is acknowledged that an improvement in motor skill performance in a clinic setting cannot translate to performance in real-world everyday tasks [10]. Stroke patients frequently exhibit problems in proprioception and balance, which are strongly linked to a fear of falling. As a result, the literature routinely assesses stroke patients’ fear of falling, claiming that this concern diminished during rehabilitation. Despite improvements in both research groups’ levels of patient fall fear, the improvement in the control group was around two times greater than in the study group. This is because so many things performed daily include several tasks in addition to the ones performed in therapy. Adding a second goal (getting points) to gait is an example of the multi-task element of daily walking activity. It causes the patient to get distracted, just like in virtual reality games. However, it is a predictable outcome that concentrating on a particular job (gait) will result in increased development of the fear of falling, just as it did in patients in the control group [7].
The cognitive task used in this study included the decision-making and verbal expression components of cognitive skills. This could be a limitation given that cognitive skills have complex domains such as memory, verbal memory, attention, spatial perception, expression, numerical functions, language, and executive functions. Additional cognitive skill components should be examined in future research [7].
Conclusions
Rehabilitation methods that include performing motor and cognitive multi-tasks simultaneously and training in conjunction with virtual environments linked to daily living activities may enhance the functional gains of stroke patients [7].
This study showed that chronic stroke patients’ gait speed, dual-task performance, functional gains, and independence improved with VR-augmented RAGT training, supporting the use of rehabilitation strategies in which VR is included concurrently with functional training. Only RAGT techniques improved functional assessments, degrees of independence, and fear of falling; hence it was assumed that this strategy could aid patients’ rehabilitation processes.
Further research is needed to determine whether combination therapy techniques are more effective for chronic stroke patients with higher cognitive involvement [7].
References
- Sisto SA, Forrest GF, Glendinning D. Virtual reality applications for motor rehabilitation after stroke. Top Stroke Rehabil 2002;8:11–23. DOI: 10.1310/YABD-14KA-159P-MN6F
- Wolfe CD. The impact of stroke. Br Med Bull. 2000;56(2):275-86. doi: 10.1258/0007142001903120
- Lund C, Dalgas U, Grønborg TK, Andersen H, et al. Balance and walking performance are improved after resistance and aerobic training in persons with chronic stroke. Disabil Rehabil 2018;40:2408–15. DOI: 10.1080/09638288.2017.1336646
- Iruthayarajah J, McIntyre A, Cotoi A, Macaluso S, Teasell R. The use of virtual reality for balance among individuals with chronic stroke: a systematic review and meta-analysis. Top Stroke Rehabil 2017;24:68–79. DOI: 10.1080/10749357.2016.1192361
- Cho JE, Yoo JS, Kim KE, Cho ST et al. Systematic Review of Appropriate Robotic Intervention for Gait Function in Subacute Stroke Patients. BioMed Res Int 2018;2018:4085298. DOI: 10.1155/2018/4085298
- Bergmann J, Krewer C, Bauer P, Koenig A et al. Virtual reality to augment robot-assisted gait training in non-ambulatory patients with a subacute stroke: a pilot randomized controlled trial. Eur J Phys Rehabil Med 2018;- 54:397–407. DOI: 10.23736/S1973-9087.17.04735-9
- Kayabinar B, Alemdaroğlu-Gürbüz İ, Yilmaz Ö. The effects of virtual reality augmented robot-assisted gait training on dual-task performance and functional measures in chronic stroke: a randomized controlled single-blind trial. Eur J Phys Rehabil Med. 2021;57(2):227-237. doi: 10.23736/S1973-9087.21.06441-8
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. DOI: 10.1016/0022-3956(75)90026-6
- Holden MK, Gill KM, Magliozzi MR, Nathan J, Piehl-Baker L. Clinical gait assessment in the neurologically impaired. Reliability and meaningfulness. Phys Ther 1984;64:35–40. DOI: 10.1093/ptj/64.1.35
- Huang HJ, Mercer VS. Dual-task methodology: applications in studies of cognitive and motor performance in adults and children. Pediatr Phys Ther 2001;13:133–40. Available at: https://pubmed.ncbi.nlm.nih.gov/17053670/