The Effectiveness of Robotic-Assisted Therapy in stroke rehabilitation

Authors: Ioana Stanescu, Irina Benedek, Oana Vanta
Keywords: upper limb rehabilitation, neurorehabilitation, robotic-assisted therapy, early stroke rehabilitation, robotic-assisted rehabilitation
Stroke remains the leading cause of disability worldwide, even though the incidence is decreasing. A cerebrovascular accident refers to an acute interruption of blood flow in the vessels supplying the brain. Therefore, it is essential to diagnose it early and treat it rapidly to reduce the risk of mortality and further impairments [1].
Robotic-assisted therapy in stroke rehabilitation has important benefits for the patients
Despite the early implementation of rehabilitation programs secondary to stroke, upper limb deficits still represent a challenge [2,3]. Consequently, the quality of life pertaining to this category of patients is affected since they cannot perform daily activities. To overcome these barriers, robotic-assisted therapies (RAT) were increasingly studied and used to improve motor deficits [4].
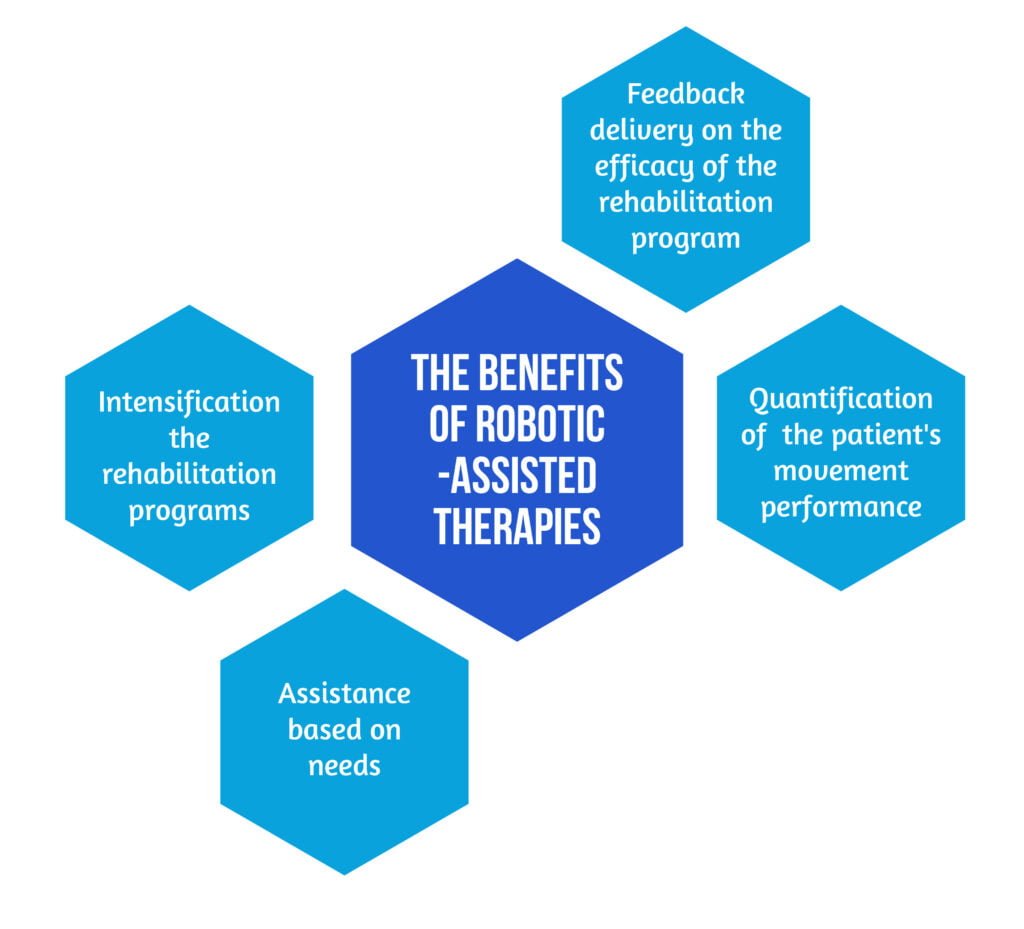
The benefits of robotic-assisted therapies are described in the Figure 1 below [2,5]:
- Intensification of the rehabilitation programs
- Assistance based on needs
- Quantification of the patient’s movement performance
- Feedback delivery on the efficacy of the rehabilitation program
Neurorehabilitation programs should be implemented as soon as possible (<6 months after stroke) when neuroplasticity is at its’ peak. Neuroplasticity refers to the ability of the nervous system to change and adapt after an injury with different possible outcomes; it has been proven that this process can be increased by active movements of the upper limb, resulting in better post-recovery outcomes [6]. Recent data also suggested that RAT could improve the execution of daily living activities if it were provided in the acute phase, not in the chronic [7]. However, two factors need to be considered when comparing RAT with conventional kinesiotherapy:
- The post-stroke stage – early versus chronic
- The amount of physical therapy that patients underwent [6].
Learn more about: Locomotion training after spinal cord injury- the physiological basis of neurorehabilitation and The effectiveness of intense neurorehabilitation of the upper limb after stroke
Robotic-assisted therapies could work as a substitution or addition to conventional kinesiotherapy
Different studies were conducted on the subject. For example, Mesiero et al. performed two randomized controlled trials where they provided robotic-assisted recovery in addition and partial substitution to conventional therapy (CT), with the same duration of treatment. They demonstrated that RAT, in addition to conventional kinesiotherapy, was more efficient than kinesiotherapy alone, while substituting it was at least as effective as CT alone [8,9].
It has been proved that RAT significantly improved upper limb motor deficits when implemented with CT. However, more data is needed to assess whether RAT alone is more beneficial than CT. Therefore, a study aimed to evaluate the effectiveness of upper limb robotic-assisted therapy in the early phase of stroke as a partial substitution for conventional therapy [10].
The research by Dehem and collabs. [10] approached RAT in the early phase of stroke in a multicentric, single-blinded, and randomized controlled study that aimed to demonstrate that adding RAT to conventional treatment for upper limb rehabilitation in the early phase of stroke will improve upper limb function, specifically dexterity and activity, and consequently social interactions of patients [10]. Participants were all volunteers and were provided with informed consent forms before they decided to enrol.
The patient eligibility criteria are mentioned in the Figure 2. below:

Patients’ recruitment started at admission to the rehabilitation center. Between May 2014 and May 2017, 262 stroke patients were evaluated, but only 45 met the criteria and agreed to participate. They were randomized according to computer generations into two groups: RAT and CT groups. Both groups underwent rehabilitation programs adapted to their needs [10].
RAT methods used in the study were reaching-type movements: the robotic device moved the patient’s paretic limb on a pre-specified trajectory. The device provided supplementary assistance on patient requests [10].
The active group received conventional therapy, which was substituted by the robotic device for 25% of the total neurorehabilitation time – in other words, 4 CT sessions of 45 minutes were replaced by RAT. In the end, both groups received comparable motor rehabilitation sessions of the same duration. All rounds were performed under the careful supervision of a specialized therapist [10].
To evaluate the results, several parameters were quantified at baseline (during the first month after stroke) (T0), after a 9-week intervention (T1), and 6 months after the cerebrovascular accident (T2). Three main characteristics were of interest: severity of upper limb motor deficits, activity limitations, and restrictions on social participation.
The evaluation scales used in this study [10] are shown in Table 1:
| ITEM MEASURED | SPECIFIC SCALES |
| Motor and functional upper limb parameters | FMA-Upper Extremity Score (FMA-UE) |
| Motor and functional upper limb parameters | Box and Block Test (BBT) |
| Activity limitation in manual functioning | Wolf Motor Function Test (WMFT) |
| Activity limitation in manual functioning | Abilhand and Activlim questionnaires |
| Quality of life | Stroke Impact Scale (SIS) |
The International Classification of Functioning (ICF) showed that the domains of motor control, manual ability, and social participation are strongly interconnected, and therefore they should be assessed in both study groups [11].
The benefits of RAT versus conventional therapy
Stroke patients were evaluated six months after stroke onset. Patients who performed RAT training sessions showed: enhanced global manual dexterity (measured by BBT), higher upper limb ability in the execution of functional tasks (measured by WMFT), and increased social participation (measured by SIS) [10].
Similar improvements were noticed in all study participants provided with conventional therapy with or without RAT regarding motor control in the upper limb, manual abilities, and activities of daily living. Gross manual dexterity was correlated with upper limb motor control and hand ability. Moreover, a more intense social participation followed improvements in ability and motor control [10].
The authors of this study highlight that the esponsiveness of patients to rehabilitation treatment was high in the early stroke phase, as showcased in Figure 3.

RAT was safe and well-tolerated by all patients regarding adverse reactions during the robotic-assisted training, despite the higher intensity of sessions [10].
The study authors explain the effectiveness of robotic-assisted training by high task-specific routines provided to the patients (moving the paretic limb along a given trajectory), the increased number of repetitions of the same task per session, and the constant feedback offered to patients, which increased their further performance. Also, the robotic device offered assistance when required by the patient [10].
Similar results were reported in other clinical studies. It has been shown that RAT, when replacing partially conventional therapy in stroke patients, was non-inferior or even superior to conventional therapy alone, the most relevant benefits being the improvement of upper limb function and ability to perform daily activities [4,7–9], better motor control and better range of motions and motricity index of the upper limb in the RAT group [12]. Moreover, higher scores for performing functional tasks after RAT treatment compared to usual rehabilitation training were demonstrated [13].
The effects of RAT treatment are persistent, as demonstrated in the Park study [14], where treatment effects are still persistent at 1.5 and 3 months after stroke, and the RAT group had better motor function [14]. In the study conducted by Dehem [10], the patients were evaluated at 6 months, and the RAT group had a tendency for better recovery in the upper limb motor function than patients treated with conventional therapy alone [10]. Another study showed that benefits still persist at 8 months, demonstrating long-term retention of better prognosis after robotic treatment [13].
The study limitations are related to the relatively small number of included patients. Also, some patients chose to continue conventional physical therapy after study termination, which could have influenced the final results.
Future endeavors
The following question arises: “Would RAT replace conventional rehabilitation therapy?”
To date, the recommendation depends on the stroke phase and the patient’s tolerance. Actual data recommend using RAT associated with conventional therapy for stroke patients in the early phase for maximal results, while RAT should be used alone in chronic stroke patients [9].
Conclusions
The study conducted by Dehem and collab. [10] is essential in stroke rehabilitation because it is real-life based, having recruited patients from rehabilitation centers in the early phase after stroke with moderate to severe motor deficits. Both conventional and robotic-assisted training was provided, and patients received rehabilitation sessions tailored to their needs. Furthermore, patient-reported outcomes, such as social participation, were assessed [10].
The authors highlight the importance of early rehabilitation training after stroke due to the fact that 75% of all participants in the study improved motor control and manual ability after completing the rehabilitation program. The training was provided for 9 weeks to consolidate the results in this study. The robotic-assisted neurorehabilitation group of patients demonstrated better results overall in the gross manual activity of the previously impaired upper limb and in social participation than the CT group for the same duration of treatment. The study authors pinpointed the advantages of using robotic devices in stroke rehabilitation: it allows higher intensity and task-specificity sessions while assisting when requested; moreover, the constant feedback provided to the patients would increase their participation and motivation during task completion. Also, the good results obtained by patients after training completion were still persistent at the final evaluation at 6 months after stroke onset [10].
Nevertheless, confirmation of RAT results awaits further clinical studies with a larger sample of patients, even though previous studies using robotic-assisted training have tried to fulfil the expectations for faster and better stroke recovery [10].
References
1. Pollock A, Farmer SE, Brady MC, Langhorne P et al. Interventions for improving upper limb function after stroke. Cochrane Database Syst Rev, 11 (2014), pp. 1-161. DOI: 10.1002/14651858.CD010820.pub2.
2. Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation, Lancet 2011; 377, pp. 1693-1702 DOI: 10.1016/S0140-6736(11)60325-5
3. Mackey J, Mensah H. The atlas of heart disease and stroke. World Health Organisation (2004), pp. 1-112. Available at: https://apps.who.int/iris/handle/10665/43007
4.Mehrholz J, Pohl M, Platz T, Kugler J, Elsner B. Electromechanical and robot-assisted arm training for improving activities of daily living, arm function, and arm muscle strength after stroke (review). Cochrane Database Syst Rev, 9 (2018), pp. 1-153 DOI: 10.1002/14651858.CD006876.pub4.
5. Pignolo L. Robotics in neuro-rehabilitation. J Rehabil Med, 41 (2009), pp. 955-960 DOI: 10.2340/16501977-0434.
6. Zhang C, Li-Tsang CWP, Au RKC. Robotic approaches for the rehabilitation of upper limb recovery after stroke. Int J Rehabil Res, 40 (2017), pp. 19-28 DOI: 10.1097/MRR.0000000000000204.
7. Mazzoleni S, Duret C, Grosmaire AG, Battini E. Combining upper limb robotic rehabilitation with other therapeutic approaches after stroke: current status, rationale, and challenges. Biomed Res Int 2017, pp. 1-11 DOI: 10.1155/2017/8905637
8. Veerbeek JM, Langbroek-Amersfoort AC, van Wegen EEH et al. Effects of robot-assisted therapy for the upper limb after stroke: a systematic review and meta-analysis. Neurorehabil Neural Repair 2016; pp. 107-121 DOI: 10.1177/1545968316666957.
9. Masiero S, Armani M, Rosati G. Upper-limb robot-assisted therapy in rehabilitation of acute stroke patients: focused review and results of new randomized controlled trial. J Rehabil Res Dev 2011; 48 pp. 355-366 DOI: 10.1682/jrrd.2010.04.0063.
10. Dehem S, Gilliaux M, Stoquart G, Detrembleur C et al. Effectiveness of upper-limb robotic-assisted therapy in the early rehabilitation phase after stroke: a single-blind, randomised, controlled trial. Ann Phys Rehabil Med. 2019;62(5):313–20. doi.org/10.1016/j.rehab.2019.04.002.
11. Stucki G, Melvin J. The international classification of functioning, disability and 469 health: a unifying model for the conceptual description of physical and 470 rehabilitation medicine. J Rehabil Med 2007;39:286–92 doi: 10.2340/16501977-0044.
12. Sale P, Franceschini M, Mazzoleni S, Palma E et al. Effects of 501 upper limb robot-assisted therapy on motor recovery in subacute stroke 502 patients. J Neuroeng Rehabil 2014;11:1–8. Doi: 10.1186/1743-0003-11-104.
13. Lo AC, Guarino PD, Richards LG, Haselkorn JK et al. Robot-assisted therapy for long-term upper-limb impairment after stroke. N Engl J Med 2010;362:1772–83.DOI: 10.1056/NEJMoa0911341
14. Park H, Kim S, Winstein C, Gordon J, Schweighofer N. Short-duration and intensive training improves long-term reaching performance in individuals with chronic stroke 2017;30:551–61.DOI: 10.1177/1545968315606990









