The positive effect of cognitive rehabilitation in early ischemic stroke

Authors: Ioana Stanescu, Oana Vanta
Keywords: stroke, cognitive impairment, rehabilitation
- The increasing incidence of post-stroke cognitive decline
- Factors influencing the cognitive decline in stroke survivors
- Assessment of cognitive functions after a stroke
- Effectiveness of cognitive rehabilitation in stroke patients with cognitive dysfunction
- Evaluation protocol
- Study results
- Conclusion
- References
The increasing incidence of post-stroke cognitive decline
Demographic changes towards an ageing population lead to increased stroke incidence, with age representing a non-modifiable stroke risk factor. By 2050, it is expected that there will be more than 200 million stroke survivors worldwide. A future increase in the burden of stroke is predicted by demographic studies, especially in patients over 75 years and in low- and middle-income countries [1]. Actually, 60% of stroke patients are older than 75 years, and half are older than 80 years. This proportion is expected to increase over the next ten years, a shift that is correlated with the ageing process [2].
The risk of cognitive impairment increases significantly both with ageing and in stroke survivors. Therefore, there is a shared susceptibility for stroke and dementia in the elderly. After a stroke, variable levels of impairment in the visual spatial function, orientation, memory, and attention may be present. Post-stroke cognitive impairment delays motor recovery and influences the prognosis. Nonetheless, cognitive rehabilitation training improves cognitive dysfunction and promotes recovery of patients’ activities of daily living (ADL) [3]. To address this need, a study conducted by Xuefang et al. [3] aimed to evaluate the role of cognitive training and motor rehabilitation in patients with cognitive impairment in the early stage after a stroke [3].
Factors influencing the cognitive decline in stroke survivors
Poststroke cognitive decline is not only related to the location and severity of the stroke but also to previous cardiovascular risk factors and patients’ socioeconomic status [3–5].
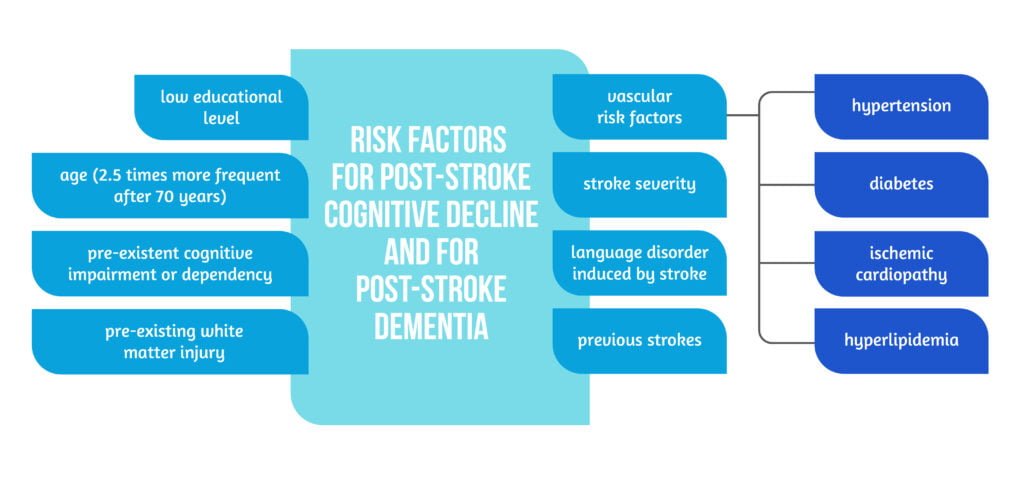
The importance of stroke-related cognitive impairment is that a relevant number of patients suffer from cognitive decline in a temporal relation to a cerebrovascular event, either prior or as a secondary outcome; thus, stroke registries were used to record the prevalence of cognitive decline impairments. Studies have shown that up to 13% of patients have a pre-existent mild cognitive impairment prior to a stroke, and 10 to 15% have prior dementia. Approximately 30% of patients have a degree of cognitive impairment after the first cerebrovascular event, while 10% will develop a more severe form of cognitive impairment, namely dementia, after the first stroke. Furthermore, more than 30% of patients develop dementia after multiple and recurrent strokes [1–2, 4–5].
Stroke impacts the risk of dementia due to the fact that the incidence of cognitive dysfunction is 6 to 9 times higher in stroke patients than in the general age-matching population [5]. In this severity type of relationship between dementia and stroke, stroke influences the brain’s cognitive reserve as the severity of the ischemic event precipitates the cognitive decline, with different severity levels of stroke decreasing the incidence age for dementia. Severe strokes will bring further the onset of dementia by 25 years, while minor strokes will precipitate the event by 4 years, and transient ischemic attacks by 2 years [4].
Patients with stroke have a 3-fold increased risk of dementia 5 years post-event compared to the general population of the same age, while patients with severe strokes experience a 47 times higher incidence of dementia [4].
Assessment of cognitive functions after a stroke
The appropriate timeframe to assess cognitive functions in ischemic stroke relates to brain plasticity. The scores on various cognitive tests could be severely modified in the acute stroke phase, gradually improving after several weeks [4]. The first three months after a stroke are considered the “golden period” for motor and cognitive recovery. Early diagnosis of post-stroke cognitive impairment has a substantial impact, establishing appropriate rehabilitation interventions. Moreover, diagnosis of post-stroke dementia is applied to patients with severe cognitive deficits persisting 6 months after the initial event [4].

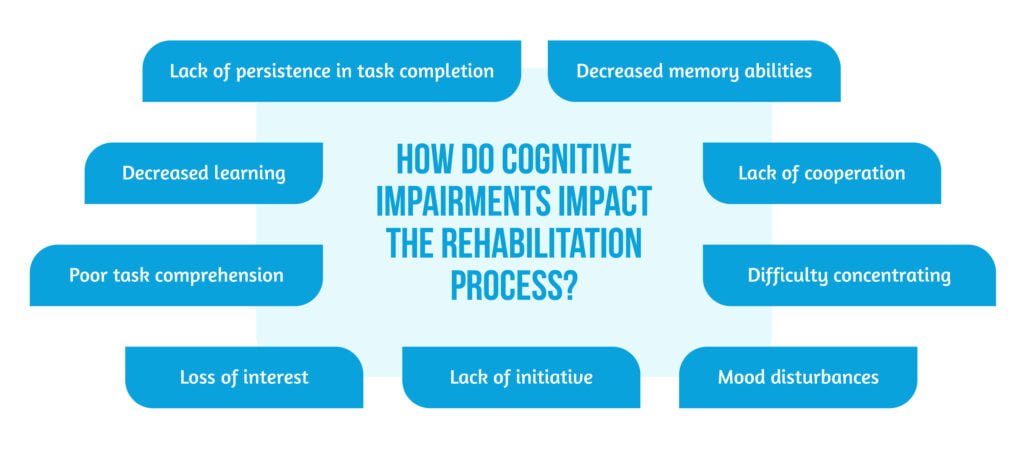
The impairments of several cognitive domains (as seen in Figure 2 above) impact the quality of life and influence the rehabilitation process in several ways ( as seen in Figure 3 below) as patients with cognitive decline after stroke will suffer from different brain lesions when conducting improper mental activities. The reduced mental activity after a stroke negatively impacts the rehabilitation process.
Unfortunately, due to brain damage, patients will suffer different kinds of cognitive impairment following a stroke [5]. As a result, different cognitive assessment tools were developed to properly evaluate the cognitive brain functions:
- Montreal Cognitive Assessment scale (MoCA)
- The Informant Questionnaire for Cognitive Decline in the Elderly (IQCODE)
- The Simple Intelligence State Examination score
- The Neurobehavioral Cognitive Status Examination score
- The Mini-Mental Status Examination (MMSE) [3,4].
Effectiveness of cognitive rehabilitation in stroke patients with cognitive dysfunction
Xuefang et al. tried to answer this question on the effectiveness of cognitive rehabilitation in patients with cognitive dysfunction following a cerebrovascular event by performing a recent clinical study on 118 patients with first incident of ischemic stroke (divided into an observational group and a control group) recruited from August 2017 to August 2019. Among them, 59 were males and 59 were females. The age was 48–76 years old, with an average of 64.2 ± 1.3 years old. The average hospital stay was 18.6±2.4 days.
The research aimed to demonstrate that adding cognitive rehabilitation training to routine motor activity and ADL training will improve cognitive and physical dysfunction after stroke and promote recovery of daily living activities [3].
Patients were considered eligible if they met the criteria described in the study’s methodology [3], which can be seen below:
Inclusion criteria for the study were:
- Clear consciousness, stable vital and neurologic signs for at least 48 h
- No history of previous mental illness
- Complete autonomy before the event
- Signed informed consent
Exclusion criteria were:
- Large cerebral infarction
- Brainstem stroke
- Presence of severe cardiac, liver, or kidney dysfunctions
- Severe infections
- Severe diabetes
- Presence of communication barriers
Study interventions on the subjects included in the observation group were performed from the third day of admission, focusing on physical rehabilitation, ADL training, and cognitive rehabilitation using computer-assisted training, as represented in Table 1 [3].

Evaluation protocol
The subjects included in the 2 study groups were clinically evaluated using the NIHSS (NIH Stroke Scale) score and cognitively, using different scales (ADL, The Simple Intelligence State Examination score, The MoCA scale, The Neurobehavioral Cognitive Status examination score) at inclusion, after 14 days and after 20 days of neurorehabilitation [3].
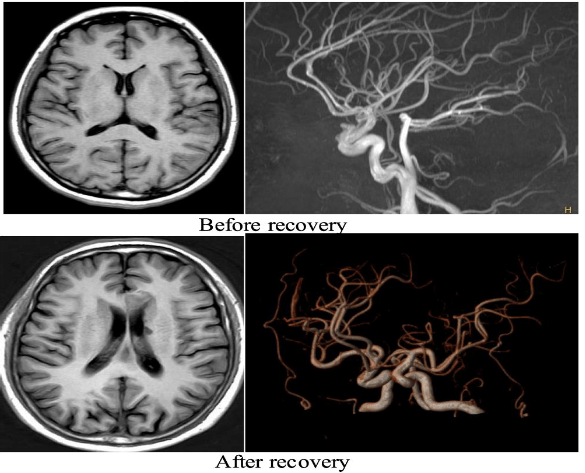
To evaluate brain integrity, other biomarkers were used. MRI images- both structural and functional, were obtained to assess lesion topography. Transcranial Doppler (TCD) was used to evaluate cerebral blood perfusion. Serum levels of specific biomarkers related to brain damage: BDNF (brain-derived neurotrophic factor), VILIP (Visinin-like protein 1), and NSE (neuron-specific enolase) were dosed [3].
Study results
The results from the study were in favour of the cognitive and motor interventions applied. In the observational group, the clinical efficacy of early cognitive rehabilitation was related to cognitive and motor functions, but also to activities of daily living [3].
An improvement in cognitive function – an increase in the MoCA scores was observed in the observational group as compared to the control group. The use of computer‐assisted cognitive training software presented patients with attractive, bright stimuli, increasing their attention and providing patients with different levels of difficulty when completing a task according to their needs. The authors believe that part of these positive results are due to the fact that the software used provided instant, objective feedback to patients [3].
An improvement in neurological function with a reduction of the NIHSS score was also observed, and a noticeable positive effect on the MRI imaging before and after treatment (see figure 4) was apparent [3]. The authors [3] considered that the mechanism behind this effect was related to the fact that occupational therapy and physical rehabilitation with exercises increase the cerebral cortex’s thickness and nutrition, and promote recovery after stroke through functional reorganization of the brain tissue [3]. Better recovery of activities of daily living was also noticed in the observation group.
Positive effects were observed on the cerebral blood flow:
- the cerebral perfusion state improved with higher blood flow velocities measured by TCD
- the serum BDNF was significantly increased
- VILIP‐1 and NSE content were significantly reduced [3].
Conclusion
The study of Xuefang et al. [3] proved that patients with cognitive impairment after a stroke benefit from early cognitive rehabilitation therapy and have an improved quality of life related to daily life activities [3].
Due to its plasticity, the brain is capable of functional reorganization and this principle provides the necessary environment for cognitive and motor rehabilitation after a stroke. Early cognitive training after a stroke creates the opportunity for the brain to relearn and improves cognitive and motor functioning, as this is an important prognostic factor in poststroke subjects.
The reserve of cognitive function after a stroke is one of the important indicators of poststroke functional prognosis; thus, both brain images and functional cognitive scores are necessary. The early identification of cognitive decline risk factors and protective factors affecting cognitive functions is essential to target specific and individual cognitive rehabilitation exercises.
References
- Béjot Y. Aging population and stroke: Red flag. Rev Neurol (Paris). 2020;176(10):751-753. DOI: 10.1016/j.neurol.2020.07.008
- Béjot Y, Bailly H, Graber M, Garnier L et al. Impact of the Ageing Population on the Burden of Stroke: The Dijon Stroke Registry. Neuroepidemiology 2019; 52:78-85. DOI: 10.1159/000492820
- Xuefang L, Guihua W, Fengru M. The effect of early cognitive training and rehabilitation for patients with cognitive dysfunction in stroke. Int J Methods Psychiatr Res. 2021; 30(3):e1882. DOI: 10.1002/mpr.1882
- Mijajlović MD, Pavlović A, Brainin M, Heiss WD et al. Post-stroke dementia – a comprehensive review. BMC Med. 2017 Jan 18;15(1):11. DOI: 10.1186/s12916-017-0779-7.
- Pendlebury ST, Rothwell PM. Oxford Vascular Study. Incidence and prevalence of dementia associated with transient ischaemic attack and stroke: analysis of the population-based Oxford Vascular Study. Lancet Neurol. 2019 Mar;18(3):248-258. DOI: 10.1016/S1474-4422(18)30442-3









