Is there any geographic variation in stroke burden worldwide?

Author: Livia Popa, Oana Vanta
Keywords: stroke burden, geographic variation, stroke risk factors
Focus Keyword: stroke belt
- What is the global stroke belt?
- Where do these differences come from?
- What is the role of major epidemiological risk factors in transnational differences in stroke disease burden?
- How do epidemiological transition, demographic shifts, and health system capacity influence the global stroke belt?
- What can society do to reduce the stroke burden and what are the global efforts to address the burden of non-communicable disease?
- Is any of this reliable? Limitations and conclusions.
- References
What is the global stroke belt?
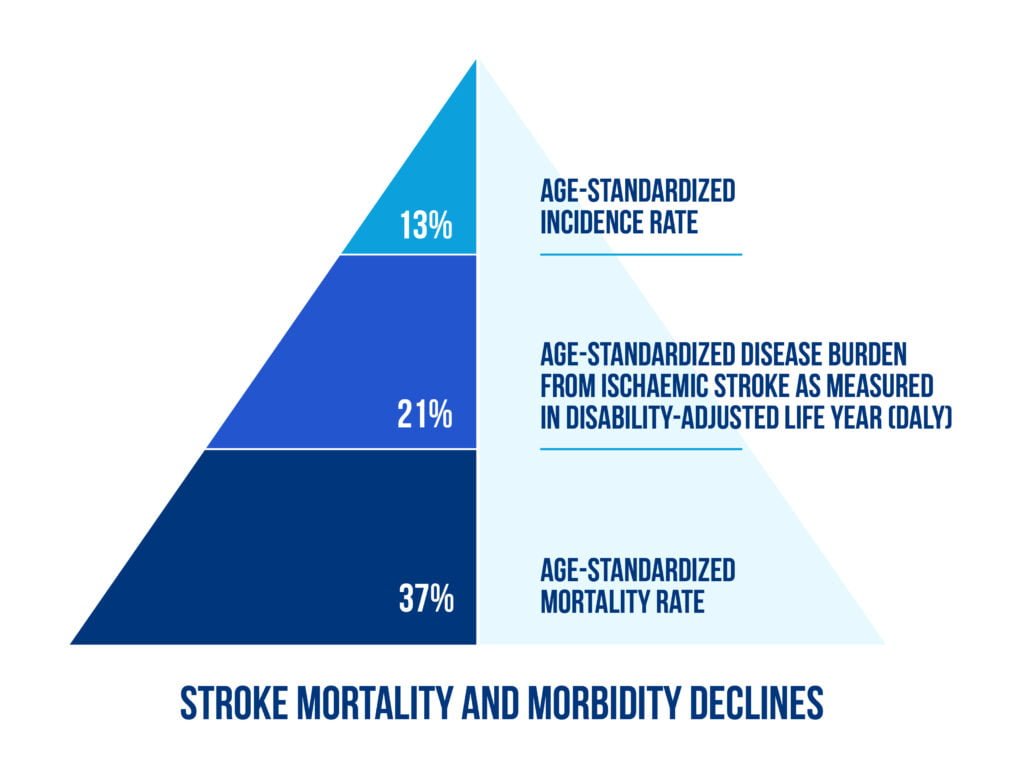
In the United States (US), stroke has been the third-leading cause of death for >70 years until 2008, the year it became the fourth leading cause of death. After five years, stroke became the fifth cause of death. As one can imagine, the stroke burden worldwide is a very serious problem. This fact shows that age-standardized stroke mortality and morbidity rates in the developed world have a sustained reduction. These improvements also translate into absolute stroke mortality and morbidity declines, as seen in Figure 1 below [1]:
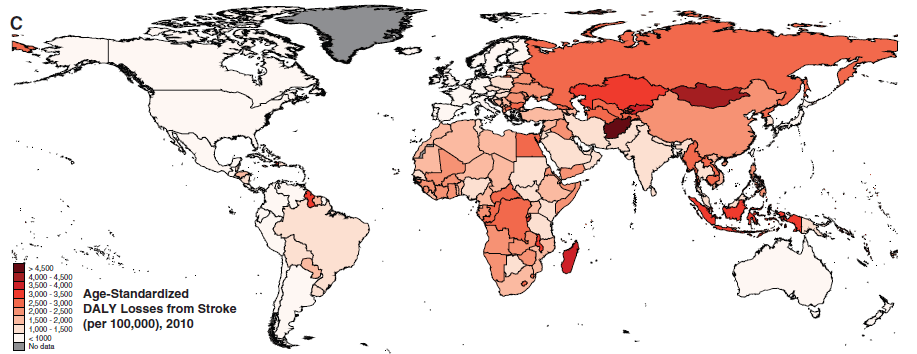
DALYs are a ‘summary measure of disease burden that combines the impact of years of healthy life lost caused by premature death with the effect of long-term disability on quality of life over time‘ [1, 2]. See figure 2:
However, worldwide there is an expanding global stroke pandemic, and by 2030 there could be almost :
- 12 million stroke deaths
- 70 million stroke survivors
- more than 200 million DALYs lost from stroke each year [1, 2].
Is this a diverging narrative? A combination of demographic, epidemiological, and health system factors in low- and middle-income countries contributed to a 100% increase in absolute stroke incidence, compared to a 42% decline in high-income countries over the same period [3].
The concept of a global stroke belt refers to the disparity in stroke disease burden focused on the developing world. The term describes the geographic differences in stroke incidence and mortality observed in the southeastern United States [2, 3].
Where do these differences come from?
Factors such as regional differences in race or ethnicity, access to care, poverty, case facility rates, vascular risk prevalence, and environmental factors were investigated [4].
Regarding the geography of disability burden from stroke, reflected in DALY loss rates, there is a similarity with the pattern for stroke mortality and incidence worldwide. The high DALY loss rates from stroke in low- and middle-income countries represent a product of high stroke incidence rates, a younger average age of stroke onset, and the differences in access to care facilities [4, 5], as may be seen in figure 3.

What is the role of major epidemiological risk factors in transnational differences in stroke disease burden?
The most important risk factor for stroke and for all-cause disease burden worldwide is hypertension, especially the type of unrecognized, untreated, and severe hypertension, which is associated with an increased risk for hemorrhagic stroke. Worldwide, the prevalence of hypertension was estimated to be 26% in 2000, with a projected increase to 29% by 2025, while in developed countries of North America, Western Europe, and Australia, there is a decline in global mean age-standardized systolic blood pressure, due to the improvements in hypertension awareness, treatment, and control [2, 6, 7].
Other major risk factors for stroke are described in Figure 4 below:
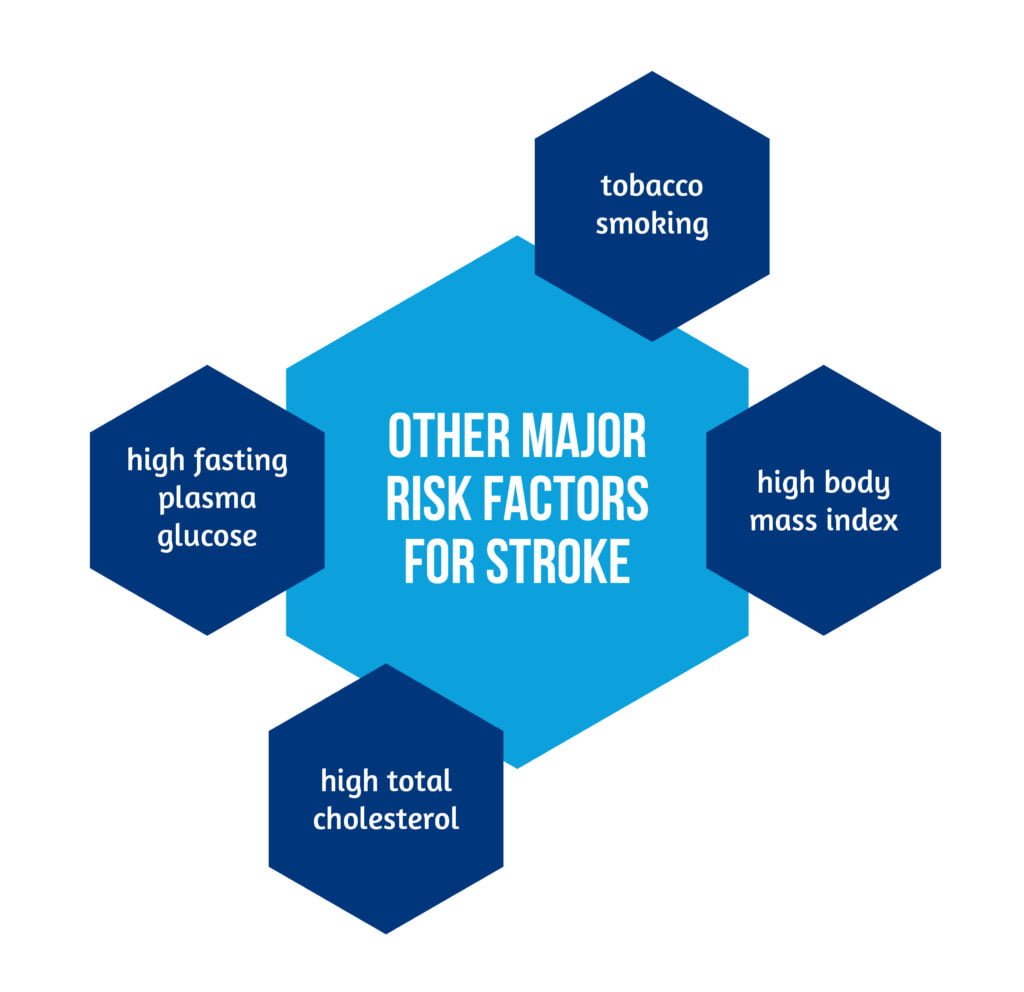
When considering high-income countries that had a high prevalence of these risk factors in the past, a positive shift is apparent in the present days, including improvements or moderation in risk factor related population measures, with the exception of obesity and diabetes mellitus. In contrast, there is an accelerating trend regarding epidemiological risk factors in low-and middle-income countries (LMIC). For example, Eastern Europe has a high absolute burden of stroke and cardiovascular disease, along with a high prevalence of high alcohol consumption, tobacco smoking, and increased body mass index, which is expected to worsen in the coming years [2, 8]. Find more details about the positive effect of cognitive rehabilitation in early ischemic stroke.
How do epidemiological transition, demographic shifts, and health system capacity influence the global stroke belt?
With the shifts in epidemiological risk factors, there is also a larger shift from infectious diseases, malnutrition, and childhood diseases to chronic conditions (e.g., cardiovascular disease and stroke). This is called epidemiological transition. With infectious diseases and malnutrition restrained, life expectancy increases and early mortality declines, but chronic diseases related to aging and epidemiological risk factors, such as stroke and cardiovascular disease, become more prevalent. Sedentarism, changes in diet facilitated by urban life, and globalization lead to an overall disease burden. Industrialization, economic development, and higher national income impact stroke mortality, incidence, and disease burden. The demographic shift and aging of the population will probably increase total stroke mortality even if the age-standardized mortality rates decline [2, 8].
Low-income countries have resource constraints for public health investments in prevention and a limited capacity for providing stroke care. Improving measures of risk factors control requires a screening capacity to identify and treat high-risk subpopulations or prevention approaches, but additional investments in public health surveillance are necessary [9].
For example, in China, stroke remains the leading cause of death and represents the predominant form of cardiovascular disease. On a national level, there is evidence of increasing mean systolic blood pressure, mean population body mass index, the prevalence of diabetes mellitus, obesity, and tobacco use. All these trends, along with aging and population growth, translate into increases in stroke incidence, mortality, and morbidity [10, 11].
What can society do to reduce the stroke burden, and what are the global efforts to address the burden of non-communicable diseases?
Some domains can be improved to influence case fatality rates and stroke morbidity. Two main scenarios can be addressed, as highlighted in Figure 5:
- Focus on prevention – increase the education about stroke and risk factors that are important for long-term prevention;
- Develop sanitary systems adapted to current needs – expand capacity for stroke treatment and recovery services (stroke units, emergency treatment, rehabilitation departments) [2].

Based on the strong association between stroke and the epidemiological risk factors, any improvements in hypertension diagnosis and treatment would have an impact on reducing stroke disease burden, and similar approaches to other risk factors such as tobacco use, diabetes mellitus, body mass index, and alcohol use may also be useful [5].
- In the beginning, the initial investments needed to address these challenges could be small (e.g., tobacco prices could be increased to reduce the cardiovascular disease burden.
- For secondary prevention, the polypill – a single pill with a combination of an antihypertensive, a lipid-lowering agent, and an antiplatelet agent – would improve adherence and reduce costs [5].
Without proper resourcing and a transnational organizing framework for developing and implementing targeted and sustained interventions, economic development alone is insufficient to reduce the absolute number of stroke-related deaths [5].
Is any of this reliable? Limitations and conclusions.
Not only at the country level but within-country or within-region, there are differences in the pattern of stroke disease burden, which may have profound and unique policy implications.
Data on stroke incidence are based on the population-based study, but in LMIC, much of the data reflects hospital data or modeling estimates due to the lack of tools in stroke surveillance data collection [12].
- The stroke epidemic is concentrated in a global stroke belt in the developing world, showcasing substantial disparities in stroke disease burden among countries and regions [12].
- Although in high-income countries there has been a reduction in age-standardized mortality and morbidity from stroke, the total disease burden from a stroke on a global basis remains substantial, particularly in developing countries [12].
- Trends in epidemiological risk factors, alongside aging and population growth in the future, are expected to increase the absolute burden of disease from stroke as part of the shift from infectious to non-communicable illnesses [2].
- To reduce the disease burden from a stroke, the focus is now on risk factors, particularly hypertension, alcohol use and tobacco use
- Investments in public health infrastructure to ensure prevention and treatment are necessary.
- Systematic epidemiological surveillance could help prioritize and target public health efforts [2].
References
- Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA et al., Global burden of diseases, injuries, and risk factors study 2010 (GBD 2010) and the GBD Stroke Experts Group. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014; 383:245–254. doi: 10.1016/S0140-6736(13)61953-4.
- Kim AS, Cahill E, Cheng NT. Global Stroke Belt: Geographic Variation in Stroke Burden Worldwide. Stroke. 2015; 46(12):3564-70. doi: 10.1161/STROKEAHA.115.008226.
- Heron, M. Deaths: Leading causes for 2008. Natl Vital Stat Rep. from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 2012;60:1–95. Available at: https://pubmed.ncbi.nlm.nih.gov/22827019/
- NCHS Data Brief. Mortality in the United States, 2013. National Center for Health Statistics Website. Available at: http://www.cdc.gov/nchs/data/databriefs/db178.pdf.
- Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009; 8:345–354. doi: 10.1016/S1474-4422(09)70023-7.
- Kearney PM, Whelton M, Reynolds K, Muntner P et al., Global burden of hypertension: analysis of worldwide data. Lancet. 2005; 365:217–223. doi: 10.1016/S0140-6736(05)17741-1.
- Centers for Disease Control and Prevention. Ten great public health achievements–United States, 2001–2010. MMWR 2011; 60:619–623. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6019a5.htm
- Howard G, Howard VJ. REasons for Geographic And Racial Differences in Stroke (REGARDS) Investigators. Ethnic disparities in stroke: the scope of the problem. Ethn Dis. 2001; 11:761–768. DOI: 10.1159/000086678
- Cushman M, Cantrell RA, McClure LA, Howard G et al. Estimated 10-year stroke risk by region and race in the United States: geographic and racial differences in stroke risk. Ann Neurol 2008; 64:507–513. doi: 10.1002/ana.21493.
- Liu L, Wang D, Wong KS, Wang Y. Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke 2011; 42:3651–3654. doi: 10.1161/STROKEAHA.111.635755.
- Moran A, Gu D, Zhao D, Coxson P et al. Future cardiovascular disease in China: Markov model and risk factor scenario projections from the coronary heart disease policy model-China. Circ Cardiovasc Qual Outcomes 2010; 3:243–252. doi: 10.1161/CIRCOUTCOMES.109.910711.
- Lim SS, Vos T, Flaxman AD, Danaei G et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8.









