Efficacy of technology-assisted gait rehabilitation in Parkinson’s disease

Authors: Ioana Stanescu, Oana Vanta
Keywords: Parkinson’s disease, gait rehabilitation, motor fluctuations, balance training
Parkinson’s disease – a frequent neurodegenerative disorder
Beforo discussing about the efficacy of technology-assisted gait rehabilitation in Parkinson’s disease we should first define this pathology. Parkinson’s disease (PD) is a progressive neurodegenerative disorder characterized by motor and non-motor symptoms; bradykinesia, rigidity, rest tremor, posture, and gait impairment are among the most common signs. PD affects 1% of the population above 60 years, and its prevalence is increasing with age from 0.5–1% among those aged between 65–69 years to 1–3% among people 80 years and older. The annual incidence is 13.5 per 100,000 people [1].
The median age of onset of Parkinson’s disease is 60 years. With an aging population, both the prevalence and incidence of PD are expected to increase by more than 30% by 2030 [2].
PD is a multifactorial disease, with both genetic and environmental factors. Among all, age is the strongest risk factor. Its pathogenesis is related to a decrease in dopaminergic transmission in the motor portions of the basal ganglia caused by the loss of dopaminergic neurons in the substantia nigra of the midbrain [3].
Gait impairment in Parkinson’s disease
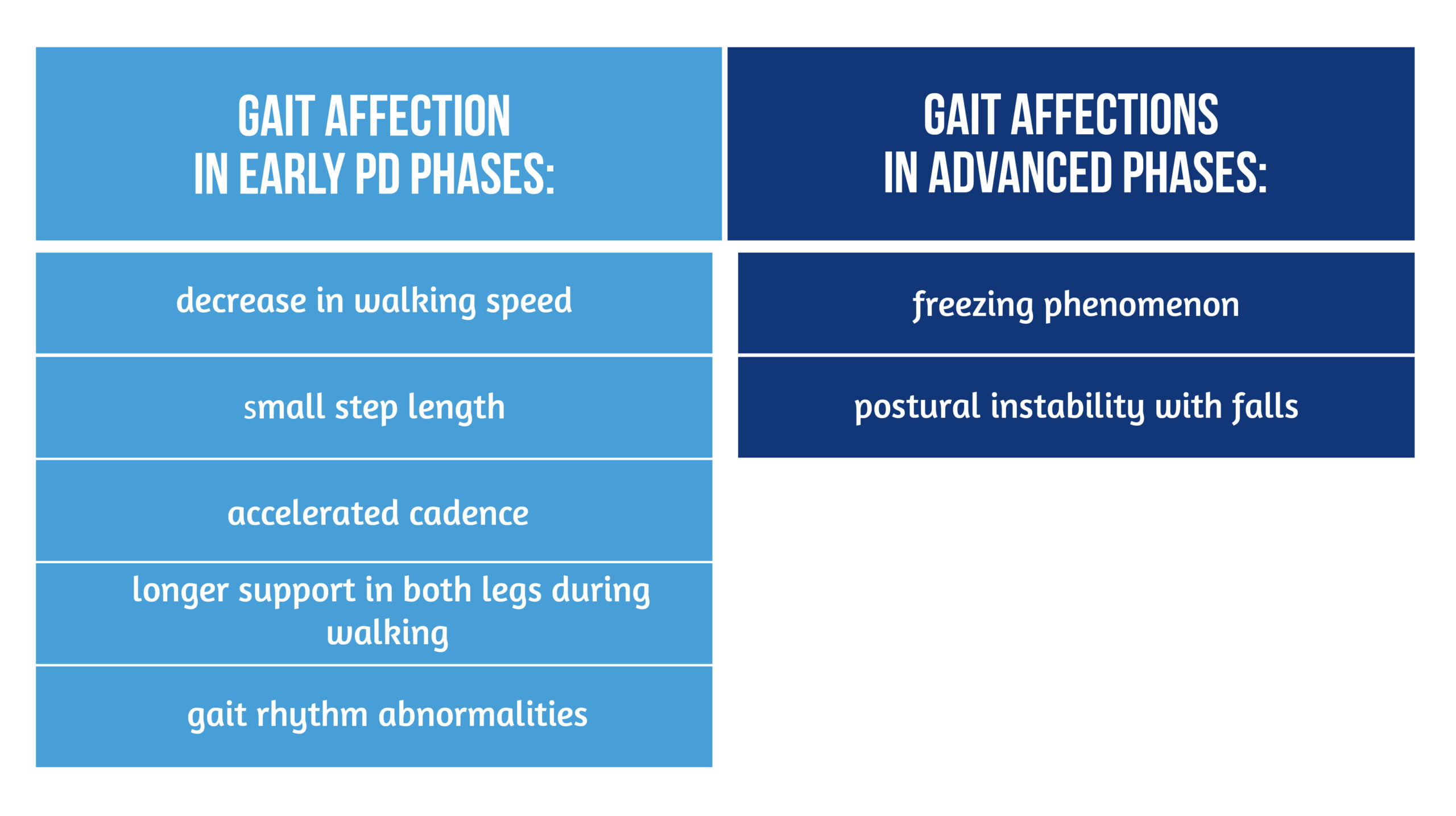
Gait impairments are among the most common and disabling symptoms of Parkinson’s disease. PD patients have modified gait patterns in both early and advanced phases of the disease. Common pathologic gait features are:
In early PD phases, gait troubles are mild, while in advanced phases, postural tone impairment and the occurrence of axial signs contribute to more severe gait troubles [4–6] (Figure 1).
Freezing of gait (FOG) is a sudden and brief episode of absence or marked reduction of foot progression despite the intention to walk. The patient is unable to move his feet, which seem to be “stuck” on the ground, with an increased risk of falling [7].
Gait impairments and other axial symptoms are poorly responsible for the dopaminergic treatment. Additional therapeutic strategies, such as neurorehabilitation, should be implemented to increase the patient’s mobility and decrease falls [8].
The efficacy of physical therapy in PD
Rehabilitation is considered an adjuvant to pharmacological and surgical treatments for Parkinson’s disease to maximize functional ability and minimize secondary complications. The rehabilitative training should be “goal-based” in PD, i.e. targeted at practicing and learning specific activities in the core areas [9].
Conventional physiotherapy significantly improved motor symptoms, gait, and quality of life. Exercise therapy in patients with Parkinson’s disease using a variety of physiotherapy interventions may improve gait, balance and flexibility, aerobic capacity, initiation of movement, and functional independence [10].
Recent meta-analyses demonstrated that rehabilitation could induce important benefits, particularly for gait and balance. Also, a systematic review of 33 randomized trials involving 1518 patients evaluated various physiotherapy interventions, including:
- general physiotherapy
- exercise
- treadmill training
- cueing
- dance
- martial arts.
Significant improvements were noticed in walking speed, endurance, step length, mobility, and balance. Also, the scores of the Unified Parkinson’s Disease Rating Scale (UPDRS), the standard scale for quantifying motor and non-motor symptoms in PD, improved with physiotherapy [11].
Technology-assisted rehabilitation training improves the gait of Parkinsonian patients
Training using electromechanical devices has been studied in neurological disorders in which gait impairment is an important and disabling feature. Technology-assisted gait training was found effective in patients with Parkinson’s disease [8,12]. The main types of devices used for gait training are treadmills and robotic systems.
Treadmill training (TT) promotes gait practice in safe conditions for the patient, as it prevents falls and other accidents. Other advantages over real-ground training include changing gait parameters according to the patient’s condition. It allows higher walking speed, longer steps, and improved balance and stability. TT showed better results in Parkinsonian patients with mild or moderate disability [12].
Robot-assisted devices have been increasingly studied in rehabilitation protocols for patients with motor deficits or gait impairments. Gait training using robotic devices has shown benefits in rehabilitating PD patients. The robot is an end-effector type and sets a longer stride length while decreasing body weight. The technique is feasible in patients with important gait and axial troubles or severe disabilities, providing intense and safer training challenges. Also, the system provides somatosensory cues during gait training [13]. Robot-assisted gait training (RAGT) is shown in Figure 2.

Treadmill training versus robot-assisted gait training in Parkinson’s disease
Italian authors conducted a prospective multicenter randomized study to compare the effects of RAGT and TT in improving the gait parameters of PD patients. They included 110 patients with at least stage 2 of PD, according to the Hoehn and Yahr scale, with walking difficulties and stable pharmacologic treatment.
Patients were allocated into 2 groups: the first group performed robot-assisted gait training, and the second group was included in treadmill training without body-weight support. Both groups completed the same duration of treatment and sessions under physiotherapist supervision [8].
All patients underwent clinical evaluation with specific tools that measured gait parameters, quality of life, and PD severity (see Table 1).
| GAIT PARAMETER | SCALES AND TESTS |
Gait endurance | 6-minute walk test (6MWT) |
Gait capacity | Time Up and Go test (TUG) 10-meter Walk Test (10MWT) |
Freezing of gait | Freezing of Gait Questionnaire (FOG-Q) |
Walking difficulty | The Unified Parkinson’s Disease Rating Scale II, item 14 Walking Handicap Scale (WHS) |
PD-related disability | UPDRS total score UPDRS parts II and III |
| Quality of life | Parkinson Disease Questionnaire-39 (PDQ-39) |
Table 1. Gait parameters assessed in the study conducted by Capecci et al. [8].
All parameters were assessed in the morning, during the “on” medication phase, at inclusion, and after 4 weeks of 5 days/week training.
The authors pinpoint that both technology-assisted rehabilitation methods effectively improve walking endurance, gait capacity, disability, and quality of life in Parkinsonian patients. However, differences were noted between the 2 techniques. Also, the walking performance score reflecting the independence of PD patients during walking improved after treatment in all patients [8].
Robot-assisted gait rehabilitation and treadmill training
The authors underlined that both methods are efficient for different gait parameters. Treadmill training improves gait endurance and capacity more than RAGT. Lack of body weight support in TT increases the training effort, leading to better endurance. TT increases gait speed and stride length and decreases hypokinesia [14].
RAGT improves gait cadence by imposing an equal stride length, providing gait symmetry. Gait velocity could be increased, and body-weight support could be variable, depending on the patient’s abilities. RAGT improved the freezing of gait score. Also, somatic and sensory feedback is provided to patients, facilitating the motor learning process [8].
Improvements in the activities of daily living were noticed after rehabilitation in the RAGT group, reflected by a decrease in the total UPDRS score.
RAGT provides more benefits than TT in the gait rehabilitation of patients who require walking assistance and those who develop gait freezing. It is possible that the constraining nature of the robotic system, which imposes a longer duration and higher training intensity, is responsible for these effects.
Conclusion | Gait rehabilitation in Parkinson’s disease
Technology-assisted gait rehabilitation is more efficient in patients with Parkinson’s disease in mild, moderate, or severe stages compared with conventional therapy. Two methods are shown to be effective: treadmill training and robot-assisted gait training. Both methods led to a significant increase in walking capacity, endurance, and walking speed. The patient’s disability is reduced, and the quality of life increases.
Moreover, robot-assisted gait training is more effective in decreasing the freezing of gait than the treadmill, while gait endurance is improved mainly by treadmill training.
Patients requiring walking assistance, with gait freezing, or severely disabled seemed to benefit more significantly from technology-assisted gait rehabilitation than conventional therapy.
For more information about neurorehabilitation, visit:
- Efficacy of placebo in managing pain for neurological disorders
- Neurorehabilitation in dystonia – a holistic approach
- Spatial memory recovery in neurorehabilitation using VR
We kindly invite you to browse our Interview category: https://efnr.org/category/interviews/. You will find informative discussions with renowned specialists in the field of neurorehabilitation.
References
- Tysnes OB, Storstein A. Epidemiology of Parkinson’s disease. J Neural Transm (Vienna). 2017 Aug;124(8):901-905. doi: 10.1007/s00702-017-1686-y.
- Kouli A, Torsney KM, Kuan WL. Parkinson’s Disease: Etiology, Neuropathology, and Pathogenesis. In: Stoker TB, Greenland JC, editors. Parkinson’s Disease: Pathogenesis and Clinical Aspects [Internet]. Brisbane (AU): Codon Publications; 2018 Dec. Chapter 1. Available at: https://pubmed.ncbi.nlm.nih.gov/30702842/
- DeLong MR, Wichmann T. Basal Ganglia Circuits as Targets for Neuromodulation in Parkinson Disease. JAMA Neurol. 2015 Nov;72(11):1354-60. doi: 10.1001/jamaneurol.2015.2397
- Boonstra TA, van der Kooij H, Munneke M, Bloem BR. Gait disorders and balance disturbances in Parkinson’s disease: clinical update and pathophysiology. Curr Opin Neurol. 2008 Aug;21(4):461-71. doi: 10.1097/WCO.0b013e328305bdaf.
- Sale P, De Pandis MF, Le Pera D, Sova I, et al. Robot-assisted walking training for individuals with Parkinson’s disease: a pilot randomized controlled trial. BMC Neurol. 2013 May 24;13:50. doi: 10.1186/1471-2377-13-50.
- Nieuwboer A, Giladi N. Characterizing freezing of gait in Parkinson’s disease: models of an episodic phenomenon. Mov Disord. 2013 Sep 15;28(11):1509-19. doi: 10.1002/mds.25683.
- Bloem BR, Hausdorff JM, Visser JE, Giladi N. Falls and freezing of gait in Parkinson’s disease: a review of two interconnected, episodic phenomena. Mov Disord. 2004 Aug;19(8):871-84. doi: 10.1002/mds.20115.
- Capecci M, Pournajaf S, Galafate D, Sale P, et al. Clinical effects of robot-assisted gait training and treadmill training for Parkinson’s disease. A randomized controlled trial. Ann Phys Rehabil Med. 2019 Sep;62(5):303-312. doi: 10.1016/j.rehab.2019.06.016.
- Abbruzzese G, Marchese R, Avanzino L, Pelosin E. Rehabilitation for Parkinson’s disease: Current outlook and future challenges. Parkinsonism Relat Disord. 2016 Jan;22 Suppl 1:S60-4. doi: 10.1016/j.parkreldis.2015.09.005.
- Radder DLM, Lígia Silva de Lima A, Domingos J, Keus SHJ, et al. Physiotherapy in Parkinson’s Disease: A Meta-Analysis of Present Treatment Modalities. Neurorehabil Neural Repair. 2020 Oct;34(10):871-880. doi: 10.1177/1545968320952799.
- Tomlinson CL, Patel S, Meek C, Clarke CE, et al. Physiotherapy versus placebo or no intervention in Parkinson’s disease. Cochrane Database Syst Rev. 2012 Jul 11;(7):CD002817. doi: 10.1002/14651858.CD002817.pub2.
- Mehrholz J, Kugler J, Storch A, Pohl M, Elsner B, Hirsch K. Treadmill training for patients with Parkinson’s disease. Cochrane Database Syst Rev. 2015 Aug 22;(8):CD007830. doi: 10.1002/14651858.CD007830.pub3
- Alwardat M, Etoom M, Al Dajah S, Schirinzi T, et al. Effectiveness of robot-assisted gait training on motor impairments in people with Parkinson’s disease: a systematic review and meta-analysis. Int J Rehabil Res. 2018 Dec;41(4):287-296. doi: 10.1097/MRR.0000000000000312.
- Muñoz A, Corrêa CL, Lopez-Lopez A, Costa-Besada MA, et al. Physical Exercise Improves Aging-Related Changes in Angiotensin, IGF-1, SIRT1, SIRT3, and VEGF in the Substantia Nigra. J Gerontol A Biol Sci Med Sci. 2018 Nov 10;73(12):1594-1601. doi: 10.1093/gerona/gly072.









